
The following article was published by the American Association of Provider Compensation Professionals (AAPCP).
Following the introduction of the Final Rules by the Department of Health and Human Services (HHS) at the beginning of 2021, VMG Health has seen a growing number of organizations prioritizing their value-based care (VBC) strategy through the creation of value-based enterprises (VBEs) and/or structuring arrangements in accordance with the safe harbor framework of the Final Rules. These value-based exceptions and safe harbors are intended to advance the transition from volume to value by allowing for more flexibility in structuring compliant arrangements. Since physicians are often the cornerstone of any VBC strategy due to their ability to drive savings and clinical quality, this added flexibility of the Final Rules has prompted many healthcare leaders to revisit and modernize their physician alignment models.
With the unwavering prominence of VBC in the market, there are already numerous alignment strategies where healthcare providers enter into value-based arrangements with physicians to improve clinical quality outcomes, coordination of care among providers and across care settings, and cost efficiencies in exchange for an incentive or bonus payment that is subject to performance metrics. In some cases, healthcare providers like hospitals and health systems are internally creating and self-funding these programs in anticipation of future changes to reimbursement. While in other cases, healthcare providers may already have payer contracts in place where they are eligible for value-based reimbursement and may want to share a portion of the incremental reimbursement and shared savings payments with the physicians who contributed to this achievement.
Regardless of the alignment vehicle, when structuring these arrangements with physicians, it is critical to ensure regulatory compliance, and one of the common themes in the Final Rules is the legitimacy of the performance metrics that will be used to trigger value-based payments. Specifically, there is an emphasis on clinical quality outcomes metrics and clinical evidence or credible medical support for these metrics. Additionally, from a valuation firm’s perspective, the credibility of the metrics is one of the primary value drivers in supporting value-based payments to physicians. The following provides insight on things to consider when selecting performance metrics for value-based arrangements and outcomes-based payment arrangements from a valuation firm’s perspective.
What to Know About Value-Based Payment Metrics
It is important to prioritize the selection of the metrics when structuring new arrangements or dusting off old arrangements. The performance metrics should be aligned with the value-based goals of the arrangement to create a meaningful and impactful program and support regulatory compliance. Additionally, from an FMV perspective, having a substantive set of metrics is a key factor in supporting or justifying value-based payments to physicians. Performing an FMV assessment helps to mitigate compliance risks and supports equitable payment models that reward physicians for their level of contribution toward achieving the value-based goals.
When it comes to determining the FMV of value-based payments to physicians, it is important to note that there is generally more flexibility if the payments can be tied to an external third party (such as effectively being funded by value-based reimbursement from a governmental or commercial payer). However, if the program is self-funded, there is generally more risk from a compliance perspective, so these programs may require more intense consideration of certain attributes of the subject program, such as the specific metrics to be utilized, to bolster support for the value-based payments.
Industry research related to value-based payment models in the market and regulatory guidance has consistently revealed the importance of key, metric-related attributes when structuring value-based payment arrangements with physicians. The following summarizes some of these key factors:
- Meaningful Number of Clinical Quality Patient Outcomes-Based Metrics
- Nationally Measured or Industry-Endorsed Metrics and Performance Targets
- Performance Targets Based on “Superior” Performance
- Difficulty Level of Achieving Maximum Payout (i.e., Stretch Goals)
- Demonstrable Physician Impact on the Metrics
Analyzing the industry research from a valuation perspective, factors such as paying for the achievement of “superior” performance standards (typically consistent with the national top decile) and selecting physician-driven, patient clinical quality outcomes metrics that are supported by credible, medical evidence can help to justify higher value-based payments to physicians.
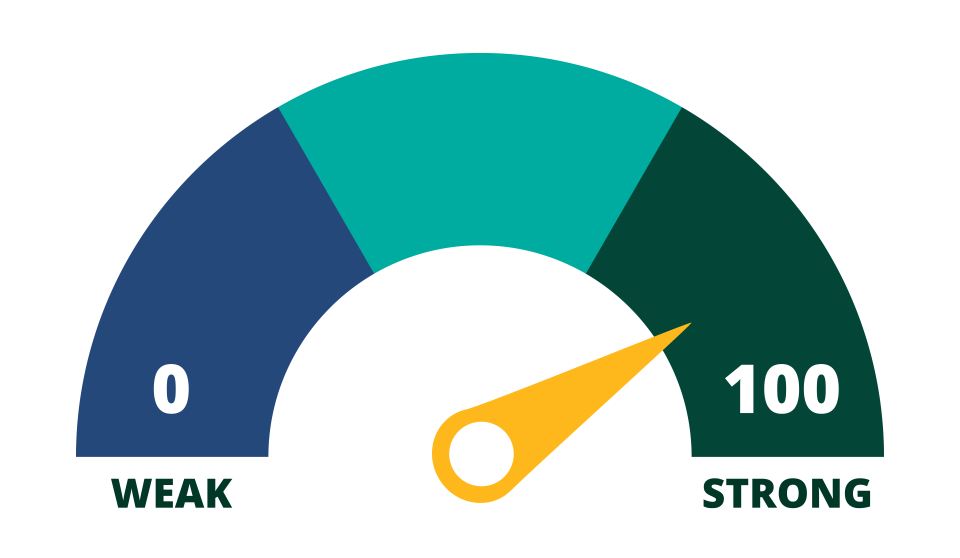
10 Questions to Help Get a Pulse on Your Metrics
Total Your Points to See How Your Metrics Score
A = 10 points
B = 5 points
C = 0 points
- Do all of the physician participants have a direct and demonstrable impact on the selected metrics?
A. Yes
B. Some
C. No
2. Has management considered the needs of the facility and/or patient population in the selection of the metrics?
A. Yes
B. Some
C. No
3. Are the selected metrics supported by credible, medical evidence for improving quality, efficiency, and patient outcomes?
A. Yes
B. Some
C. No
4. Do the selected metrics overlap with or duplicate any services required under medical staff bylaws and/or other arrangements?
A. No
B. Some
C. Yes
5. Has management established meaningful performance targets for each metric that are difficult to achieve or based on a material improvement from baseline performance (i.e., stretch goals versus maintenance goals)?
A. Yes
B. Some
C. No
6. Is achievement of the selected metrics expected to improve your organization’s performance under value-based arrangements with payers (i.e., will it generate value-based reimbursement for your organization from payers)?
A. Yes
B. Some
C. No
7. Is achievement of the selected metrics expected to generate quantifiable savings on the total cost of care for your organization or for payers?
A. Yes
B. Some
C. No
8. Are the selected metrics outcomes-based (i.e., patient clinical quality outcomes)?
A. Yes
B. Some
C. No
9. Are the selected performance targets for each metric sourced from industry-recognized or national databases (versus internally derived or self-created)?
A. Yes
B. Some
C. No
10. Are the maximum performance targets for each metric consistent with or better than what is considered “superior” level of performance (often consistent with national top decile)?
A. Yes
B. Some
C. No
This article is not intended to be, nor should it be used as, a substitute for legal, valuation, or regulatory advice.
Sources
85 Fed. Reg. 77492 (Dec. 2, 2020) (CMS Final Rule); 85 Fed. Reg. 77684 (Dec. 2, 2020) (OIG Final Rule).





