
Written by Anthony Domanico, CVA and Ben Minnis, CVA
The following article was published by the American Association of Provider Compensation Professionals.
In the rapidly evolving landscape of healthcare, traditional fee-for-service (FFS) reimbursement models are being replaced by alternative payment models that focus on value-based care in addition to, or even sometimes fully in replacement of, fee-for-service reimbursement. This shift from volume to value necessitates a strategic rethinking of compensation plans for healthcare providers to align incentives, optimize patient outcomes, and maximize revenue. The implementation of value-based compensation plans requires a deep understanding of the intricacies of different alternative payment models and the development of innovative strategies to ensure financial success while prioritizing quality care.
The Paradigm Shift: Value-Based Care and Alternative Payment Models
A key tenet of value-based care is the focus on delivering high-quality healthcare outcomes to patients while managing costs effectively. Alternative payment models, such as bundled payments, accountable care organizations (ACOs), and capitation, incentivize providers to prioritize preventive care, care coordination, and patient engagement while reducing unnecessary or inappropriate services.
These models differ from traditional fee-for-service, which rewards the quantity of services delivered rather than their outcomes. Under a fee-for-service reimbursement model, the more you do, the more you get. This is the case even if certain types of care or services are not warranted, are considered excessive based on the problem set presented by a particular patient, or do not lead to good patient outcomes.
However, under value-based contracts providers are rewarded not for the volume of services rendered, but for providing high-quality care to a large population of patients while also reducing unnecessary and/or inappropriate services.
The Compensation Shift: Designing Physician Compensation Programs to Maximize Revenue
While all value-based care models pay for value in some respect, the way various payment programs are structured will determine what compensation mechanism(s) will lead to better outcomes for both the physician and the organization.
Consider the following scenarios that are all focused on a hypothetical organization with $100 million of revenue and 200 FTE doctors ($500,000 in revenue per FTE).
Fee For Service + Value
Under a non-capitated value-based model where the organization continues to earn reimbursement under an FFS construct, with additional revenue opportunities through quality incentives, that organization might see $90 million of FFS revenue for the same book of business. In addition, that organization can earn up to an additional $20 million in value-based payments for a total possible range of $90-110 million of revenue.
Under this reimbursement structure, the organization will still be incentivized to have its physicians rewarded for productivity. After all, a sizable portion of the organization’s revenue, and most of the organization’s ability to increase the revenue pool (the $90 million), is through FFS reimbursement. As such, a compensation model under this construct might be a productivity model (with or without a base salary component). Also, it would include an additional incentive opportunity for value-based arrangements based on the metrics included in the organization’s value-based contracts.
Fee For Service + Value + Shared Savings
Another emerging component of value-based contracts is shared savings opportunities. If an insurer typically incurs costs of $10 million for managing a population of patients, and the subject organization can take high-quality care of the same population of patients for $9 million, insurers are increasingly sharing a portion of the cost savings back to the providers/health systems that are helping to achieve these savings.
Designing compensation arrangements to maximize shared savings opportunities is much trickier than under FFS and value models. After all, it is much more challenging to define metrics around achieving cost savings on a targeted population of patients than it is to measure things like hemoglobin A1c scores. As a result, we often see organizations either use shared savings dollars earned from insurers to fund larger quality incentives or pass through a portion of those earned dollars received from insurers to network physicians.
The latter option is complex in that it requires organizations to understand how those cost savings are achieved and to be able to allocate those savings earned down to the individual physician level or develop a proxy formula to estimate these factors for payment. As an example, we may see an organization decide to withhold 50% of funds earned to cover the additional costs incurred by the employer (such as hiring care coordinators to ensure patients with diabetes are getting back to the clinic for follow-up tests, etc.), and distribute the remainder by using a formula based on quality, wRVUs, or some other distribution formula.
Ensuring compensation remains consistent with fair market value under these types of arrangements is challenging. With that in mind, you will want to ensure you are working with counsel and a compensation design/valuation expert to ensure any compensation models remain consistent with fair market value.
Capitation
At the other end of the volume-to-value spectrum are capitation models which include an organization that receives a fixed payment on a per member per month basis for all members under its care. Under these models, if those 200 FTE physicians manage a panel of 50,000 patients, and the organization is reimbursed $166.67 per patient per month, that organization receives a total annual payment of $100 million.
Under these models, the organization receives a fixed payment regardless of its costs, assuming it has the same number of patients. An organization can only increase top-line revenue through growth in the patient population served, so compensation models tend to be a combination of fixed and variable. Specialists might be paid on a salary-type model (with or without incentives), while primary care providers might be paid on an acuity-adjusted panel size model whereby physicians are incentivized to take on more patients and grow the total capitated revenue of the organization.
These models may also include incentive payments tied to care coordination, quality outcomes, cost controls/reductions of unnecessary or inappropriate services, and the like.
Conclusion
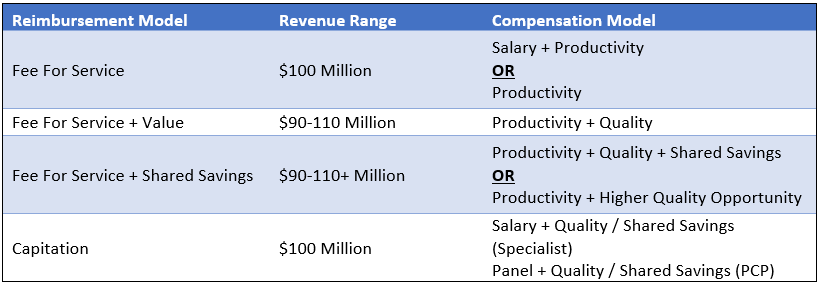
The table below summarizes the options discussed. Note that the compensation models in the right-hand column are the most predominant compensation model structures for a particular reimbursement model. However, other models may be more appropriate depending on the facts and circumstances impacting the subject organization.
Transition Strategy
In addition to designing compensation models that allow for maximum revenue potential, organizations must enact robust change management processes to ensure their providers are not lost in the transition to a new compensation model. Providers need to understand the rationale behind the new models and how their efforts contribute to both patient care and financial success for the organization and the providers. Regular feedback loops and performance evaluations can help providers track their progress and make necessary adjustments.
Conclusions and Key Takeaways
As healthcare continues to shift toward value-based care, designing an effective compensation plan is becoming increasingly crucial for provider organizations to thrive under these alternative payment models. The suitable model for your organization might vary significantly from the compensation structure observed at the neighboring health system. This is especially true considering both organizations could be positioned at distinct points along the risk continuum.
The key success driver is for organizations to design models that will help them be successful wherever they are on the continuum. By aligning incentives with patient outcomes, leveraging innovative strategies to provide more cost-effective care, and adapting to changing market dynamics, organizations can optimize revenue and physician-earning opportunities while delivering high-quality care to their patients.






