In 2010, the Centers for Medicare and Medicaid Services (“CMS”) dealt cardiologists a significant cut in technical reimbursement for their primary in-office ancillary services (such as echocardiography, nuclear medicine, etc.). Further, CMS eliminated lucrative consultation codes replacing them with lower-reimbursed E&M codes. Given these reimbursement cuts, it would seem logical to observe a decline in cardiology compensation levels across the country. Surprisingly, the opposite is true – overall compensation for cardiologists is actually on the rise. This article attempts to illustrate the compensation movement and some of the basic factors contributing to this counterintuitive trend.
Reimbursement Trends
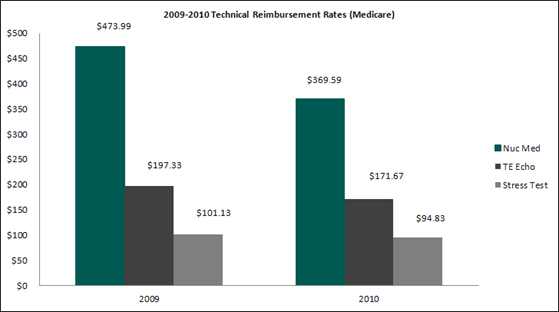
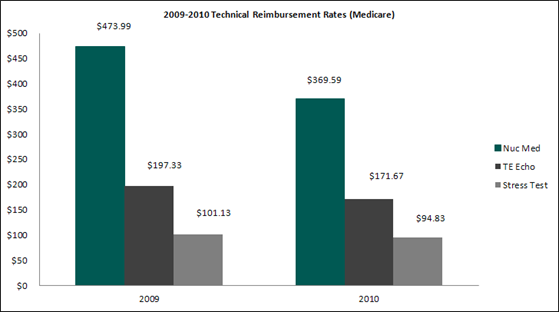
The following provides a year-over-year summary of selected technical reimbursement rates from Medicare illustrating the overall decline in cardiology reimbursement (2009 versus 2010).
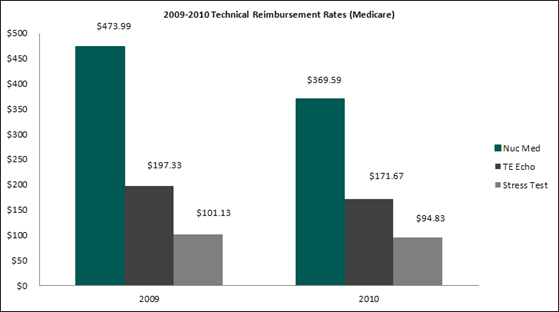
As shown above, nuclear medicine reimbursement[1] experienced the largest decline at 22%, with echocardiography[2] at 13% and cardiovascular stress test[3] at 6.2%. Please note that the chart above represents a snapshot of certain procedure-level reimbursement declines and is not meant to be an exhaustive description.
Compensation Trends in Cardiology
To illustrate compensation trends, three national surveys were considered for the specialties of noninvasive cardiology and interventional cardiology.[4] It is important to note that compensation data reported in the surveys was one-year old when the survey was published. As such, compensation data from the 2011 surveys represents compensation from the 2010 calendar year. The following provides an overview of the cardiology compensation trends observed:
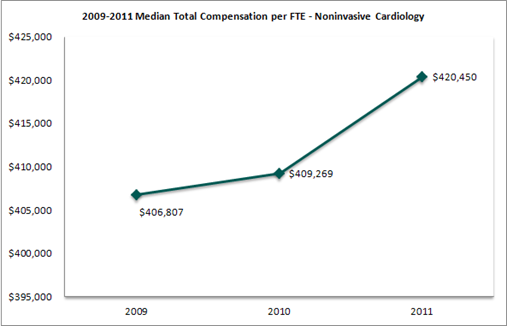
Median compensation per FTE for noninvasive cardiology increased 2.7% in the 2011 surveys (based on 2010 data) while median compensation for interventional cardiology increased 3.4%. Even more interesting is both specialties experienced moderate to no growth in compensation in the 2010 surveys (based on 2009 data) compared to the 2009 surveys (based on 2008 data).
Compensation per work relative value unit (“work RVU”) trends were also examined.
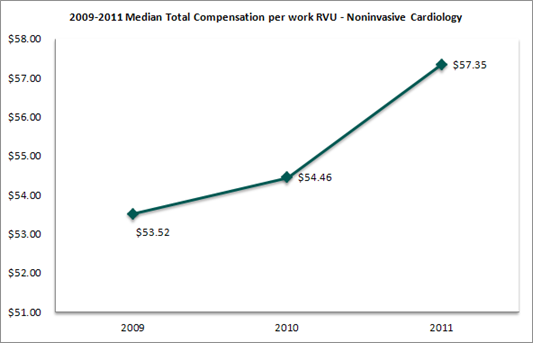
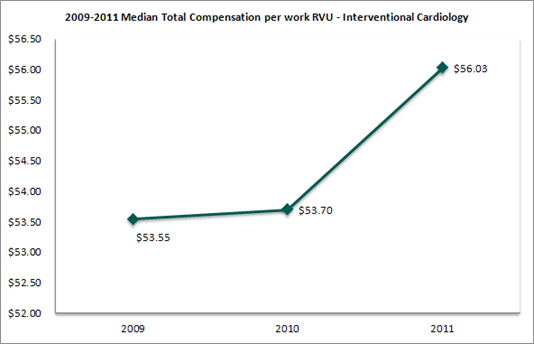
The trends in compensation per work RVU were nearly identical to those observed in total compensation per FTE. Further, the increase in compensation per work RVU would indicate that cardiologists have been paid more dollars per unit of clinical productivity.
What is Driving the Increase in Compensation?
Many factors have and continue to influence the increase in cardiology compensation. Although not a comprehensive list, the following identifies a few likely reasons:
• Supply/Demand for Cardiologists: Although cardiologists may be incentivized to integrate with hospitals, hospitals also need cardiologists to provide emergency department coverage and/or to fill community physician shortages. To meet demand, Hospitals may pay compensation rates based on published survey data for the cardiology services.
• Market Survey Data Bias: In integrating with cardiologists, most hospitals will base employment and contract compensation rates on published survey data, which is usually (at best) one-year old. Since the data is not “forward-looking” in nature, it fails to reflect the expected changes in reimbursement and the impact reimbursement declines should have (all else equal) on net compensation.
• Compensation Model Structure: Compensation per work RVU models remain prevalent in the market and are often the model of choice for hospital-cardiology integration. Work RVU models are “payor-blind” and do not contemplate local reimbursement or operating expenses (key factors in private practice compensation).
• Stacking of Services: Under hospital employment or contracting arrangements, cardiologists are often given the opportunity to provide additional services (i.e., services are “stacked” within an agreement). These services may include call coverage, medical directorships, and/or quality improvement, among others. Compensation for these services is often paid “in addition to” the compensation for clinical services.
Conclusion
Despite the hefty cuts in reimbursement implemented by CMS in 2010, cardiology compensation trends continue to show an overall increase. Hospital demand for cardiology services, strategic hospital-physician integration, the use of market survey data, and an increase in the overall services provided are factors that have (in part) played a role in the increase in cardiologist compensation.
[1] Based on CPT code 78452 (previously 78465, 78478, and 78480)
[2] Based on CPT code 93306
[3] Based on CPT code 93015
[4] Compensation surveys considered included the 2009, 2010, and 2011 editions of the MGMA Physician Compensation and Production Survey, the AMGA Compensation and Financial Survey, and the Sullivan Cotter and Associates Physician Compensation and Productivity Survey.





