
On November 21, 2025, the Centers for Medicare & Medicaid Services (CMS) released the calendar year (CY) 2026 Hospital Outpatient Prospective Payment System (OPPS) and ambulatory surgery center (ASC) payment system policy changes and payment rates final rule. In the CY 2024 OPPS/ASC final ruling, CMS finalized its proposal to continue to align the ASC payment system using the hospital market basket update, rather than the Consumer Price Index for All Urban Consumers (CPI-U) for an additional two calendar years through 2025. Further, for this CY 2026 final rule, CMS finalized its proposal to extend the utilization of the hospital market basket update as the update factor for the ASC payment system one additional year through CY 2026.
CMS finalized the update to the OPPS payment rates in line with the hospital market basket update, resulting in overall expected growth in payments equal to 2.6% in CY 2026. This increase is determined based on the projected hospital market basket percentage increase of 3.3%, less the multifactor productivity (MFP) reduction of 0.7% mandated by the Affordable Care Act. This is an increase of 0.2% from the proposed rule. In an official American Hospital Association (AHA) statement on the CY 2026 OPPS final rule, Ashley Thompson, Senior Vice President of Public Policy Analysis and Development for AHA commented:
“The AHA is disappointed that CMS has finalized cuts to hospitals and health system services, including those in rural and underserved communities. Combined with its continued inadequate market basket updates, the agency is exacerbating the challenging financial pressures under which hospitals are operating to serve their patients and communities.”
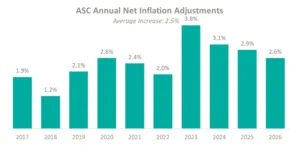
Presented in the chart below is a summary of the historical net inflation adjustments for CY 2017 through CY 2026. The annual inflation adjustments already reflect additional adjustments, such as the MFP reduction, outlined in the final rule for the respective CY. The CY 2026 inflation adjustment is slightly lower than the increase we observed last year, following a declining trend since 2023, despite inflationary increases, continued rise in labor and supply cost pressures, and recent increases in anesthesia costs.
Aligning with CMS’ view that clinical practice has shifted enough that many surgeries previously performed only in a hospital setting can now be done safely on an outpatient basis, CMS is finalizing its proposal to phase out the Inpatient Only (IPO) list. The list will be phased out over a three-year period, beginning with the removal of 285 procedures—which are mostly musculoskeletal. Phasing out the list allows Medicare to cover these procedures in outpatient settings when clinically appropriate, giving physicians more flexibility in choosing the best site of care and potentially lowering out-of-pocket costs for patients.
CMS finalized the addition of 289 surgical procedures to the ASC Covered Procedures List (CPL) for CY 2026. Additionally, CMS added 271 of the codes removed from the IPO list to the CPL. These codes correspond to procedures that have few to no inpatient admissions and are widely performed in outpatient settings, allowing clinicians greater discretion in determining site of service and giving patients more options for where to receive care.
Included in the procedures added to the CPL are cardiac ablation procedures. Cardiology advocates like the American College of Cardiology and the Hearth Rhythm Society have advocated for allowing ablation services to be performed in an outpatient setting earlier this year. Joe Sasson, Chief Commercial Officer and Senior Vice President of Ventures at MedAxiom, commented in January:
“Hopefully, those will be reimbursed by CMS (the U.S. Centers for Medicare & Medicaid Services) and others, starting in ’26 or maybe ’27. We hope for ’26.”
Also notably included are lumbar fusion spinal codes and vascular embolization or occlusion codes.
CMS projects a roughly $450M increase in total ASC payments for 2026, for an estimated total of $9.2 billion. The source of the increase in payments is a combination of enrollment, case-mix, and utilization changes.
In conclusion, we continue to see the trend of rising labor and supply costs play out through 2025 and into the finalization of the CY 2026 payment system. CMS has made strides in transitioning to eliminating the IPO list and expanding the CPL list, which was received well by major players in the industry. As Ambulatory Surgery Center Association CEO Bill Prentice points out,
“CMS acknowledges in this rule that ASCs can provide safe care to many more beneficiaries for a much wider range of procedures than is currently available… While more work is needed to address structural payment issues that limit surgery centers’ ability to perform certain procedures, Medicare beneficiaries will greatly benefit from the finalized policies in this rule.”
Overall, the final rule reflects the ongoing tension in healthcare between controlling costs and expanding access. While Medicare payment rates continue to rise, driving higher costs in the system, the industry has generally welcomed key policy changes. The phased elimination of the IPO list and the expansion of the CPL provide greater flexibility for physicians to determine the most appropriate site of care and allow more procedures to be safely performed in outpatient and ambulatory settings. These changes are seen as a step toward greater efficiency, lower out-of-pocket patient costs, and broader access to care, particularly in high-demand surgical specialties. However, as costs continue to climb, stakeholders will be watching closely to balance financial pressures with clinical appropriateness and patient safety in the evolving outpatient landscape.
![]()
Now is the ideal time to assess how CMS updates may impact your organization’s reimbursement, operations, and growth opportunities. Reach out to VMG Health’s industry experts to ensure your ASC or outpatient program can adapt to—and capitalize on—these shifts in 2026 and beyond.







