
Written by Dylan Alexander, CVA and Gerrit Elzinga, CVA
As of January 2024, Definitive Healthcare reports that there are over 338,000 physician group practices in the United States. In an independent physician practice, shareholder physicians typically take home all earnings of their business and have discretionary expenses. The compensation package of the shareholder physicians negotiated during a transaction often differs from the compensation structure of the practice pre-transaction and should be taken into consideration in the valuation of a physician practice. An inverse relationship often exists between physician compensation and the valuation of independent physician groups. This means that higher post-transaction physician compensation results in less available earnings for the practice owners to sell, ultimately leading to a lower valuation for the physician practice. Post-transaction physician compensation structure plays a significant role in the value of physician practices.
There are many forms of physician compensation. Here are a few of the most common types:
- Salaries: base salary, year-end/productivity bonuses, and guaranteed payments
- Benefits and Payroll Taxes: medical insurance, PTO balances, payroll taxes, 401(k) match, HSA, FSA, and life insurance
- Discretionary Expenses: car allowances, cell phones expenses, and travel and entertainment expenses
- Other Compensation: profit sharing, cash balance plans, medical directorships, and distributions
Physician compensation levels vary from practice to practice. As previously mentioned, shareholder physicians typically take home all practice earnings; therefore, the post-transaction compensation structure will determine whether the subject practice has earnings or compensation to monetize in a transaction. Numerous factors determine whether physicians have compensation available to sell. Productivity and reimbursement are the main components for driving fee-for-service revenue at a physician practice. Practices with productive physicians, favorable reimbursement, and ancillary service offerings generate higher revenue, which results in increased profitability. Furthermore, practices that effectively leverage mid-level providers tend to have greater profitability than those that do not, as mid-level providers deliver many of the same services at a fraction of the cost. Expense management is key; a practice overburdened with operating expenses will be less profitable. For certain practices, historical physician compensation and its attributes may not leave meaningful earnings to sell.
Impact on Valuation Methods
Physician practices are most often valued utilizing three methodologies: income approach, cost approach, and market approach. The income approach considers the future earning potential of a physician practice and discounts the projected cash flows back to its present value. The value of a physician practice is sensitive to the total amount of physician compensation and how that compensation is structured. The greater the physician compensation, the lower the projected free cash flows will be. Ultimately, a high level of post-transaction physician compensation results in a lower valuation for the practice. Conversely, lower levels of post-transaction physician compensation create increased projected free cashflows. However, total compensation should be consistent with market levels. If the compensation structure is below market, there are sustainability risks associated with retaining and recruiting new physicians after the transaction. Setting physician compensation in line with the market for physicians with similar productivity can mitigate these risks.
The market approach compares an individual practice to similar physician practice transactions in the market through the application of an earnings multiple. Practice transactions often use the application of earnings before interest, taxes, depreciation, and amortization (EBITDA) multiples. It is important to note that EBITDA is calculated after taking into consideration the post-transaction structure for all providers. The multiple is determined based on a review of similar transactions in the marketplace, attributes specific to the practice, market factors, and on perceived risk of practice profitability amongst other factors. As illustrated below, physician compensation impacts the market approach similarly to the income approach—the greater the physician compensation, the lower the earnings for which to apply an earnings multiple.
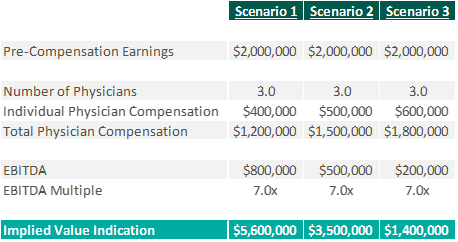
If too much physician compensation is sold, the market multiple may need to decrease to account for physician sustainability risk. Low levels of physician compensation in relation to productivity can lead to physician attrition.
The cost approach is an asset-based approach that analyzes an entity’s tangible and identifiable intangible assets. A level of post-transaction physician compensation that is consistent with the historical amounts or higher may eliminate positive future cash flows, causing the practice to be valued based on its assets versus earnings. It is not uncommon for practices to be valued using the cost approach due to the lack of attributes enabling them to monetize compensation while being consistent with market levels of compensation post-transaction.

Conclusion
Physician practices have the unique freedom to determine the services they provide, who provides those services, and how physicians can be compensated. There are multiple factors that determine the profitability of a physician practice, which directly impacts physician compensation. The amount of compensation and the way it is structured can have material impacts on the value of a practice, regardless of valuation approach. It is imperative to understand the link between post-transaction physician compensation and the fair market value of a physician practice for both buyers and sellers.
Sources
Definitive Healthcare. (2024). Number of physician group practices by state. Healthcare Insights. https://www.definitivehc.com/resources/healthcare-insights/number-physician-group-practices-by-state#:~:text=According%20to%20our%20database%2C%20there,them%20access%20to%20more%20patients
Kelleher, S. (2023). Understanding Physician Compensation Models. Health eCareers. https://www.healthecareers.com/career-resources/residents-and-fellows/understanding-physician-compensation
PayrHealth. (2022). Ancillary Services in Healthcare: Finding the Right Level for Your Practice. Managed Care Contracting Blog. https://payrhealth.com/resources/blog/list-of-ancillary-services-in-healthcare/






