
The CPC+ Initiative
In April of 2016, the Center for Medicare and Medicaid Services (CMS) unveiled the Comprehensive Primary Care Plus (CPC+) initiative. It’s the largest investment in primary care transformation to date as part of the shift towards value-based reimbursement (VBR). This reform program is an extension of the Comprehensive Primary Care (CPC) initiative that launched four years ago and is set to end December of this year. As of October 2015, over 400 primary care practices were participating in CPC encompassing eight states: Arkansas, Colorado, New Jersey, New York, Ohio, Kentucky, Oklahoma and Oregon1. As new payment models evolve, appropriately determining fair market value (FMV) for physician compensation will remain a challenge for healthcare executives.
At face value, the CPC+ initiative is meant to accommodate practices at different levels of readiness for this transformation. Track 1 is targeted towards practices seeking to start providing comprehensive care, whereas Track 2 is a hybrid model that focuses on care provision and prevention outside of the traditional face-to-face encounter, including telemedicine visits or longer visits for patients with complex needs2. The overall focus on better established relationships (payor and payor, doctor and patient) will help strengthen the quality and efficiency of care.
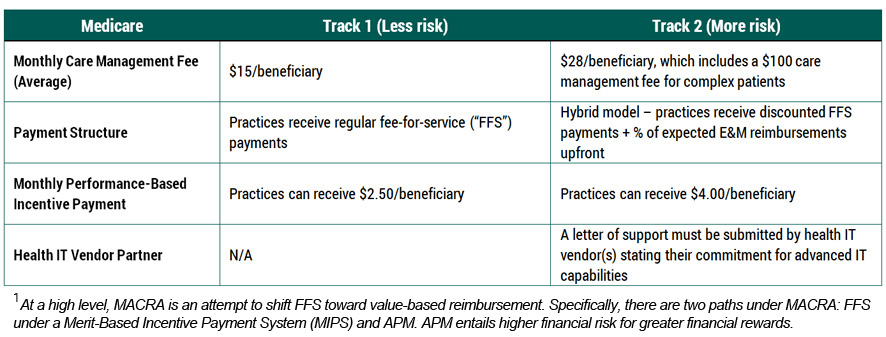
CPC+ is expected to involve up to 5,000 practices and 20,000 physicians in 20 regions (amounting to over 25 million patients) throughout its five-year plan starting January 20173. Providers can participate in CPC+ under two tracks, which will both provide a monthly care management fee and upfront performance-based incentive payments (latter of which is subject to return at year end if certain quality and utilization standards are not met). Although not confirmed at this time, CPC+ may be considered an alternative payment model (APM) under the Medicare Access and CHIP Authorization Act of 2015 (MACRA)1 4. Please refer to the chart below detailing the key differences between the two tracks5:
CPC+ will target on meeting five crucial functions:
- Access and Continuity Support (24/7 access to care and health information);
- Care Management (focus on patients with serious, chronic or multiple medical conditions);
- Comprehensiveness and Coordination (better transitions and information exchange);
- Patient and Caregiver Engagement (more interaction with patients and their families); and
- Planned Care and Population Health (prevention treatment plans).
Physician Compensation Impact and FMV
Historically, many of the items conducted by primary care physicians have not been compensated, such as time spent coordinating care on the phone, talking to social workers or conferring specialists. With the CPC+ initiative, some, if not most of these activities would be inherently embedded into the monthly care management fee.
As such, when determining the FMV of physician compensation, monthly care management fees and any types of upfront fees should be taken into consideration. For regulatory purposes it is crucial for healthcare arrangements to establish FMV correctly, which is generally defined as the price in which well-informed parties would exchange services, absent the consideration of referrals.
A typical clinical compensation analysis traditionally relies primarily on the subject provider’s production and operating cost model against the benchmark of national market surveys. With the addition of the aforementioned fees, adjustment to survey data and/or understanding market data for similar fees will need to be considered. Therefore, the traditional survey benchmarking to determining physician compensation may need to be reevaluated.
The Big Picture
With the CPC+ not in effect yet, it is hard to gauge the market sentiment and its impact on physician compensation and the process to establish FMV. Currently the CPC+ proposal demonstrates CMS’ further attempts to transition from FFS to value-based care. As more alternative payment models are introduced and market survey data lags behind, appropriately determining FMV for physician compensation will be challenging.
Footnotes:
1 “CMS Escalates Primary Care Reform”, Health Leaders Media, April 18, 2016
2 “Obamacare tests new payment system for primary care”, United Press International, April 12, 2016
3 “Red tape may tank new CMS primary-care payment model”, Modern Healthcare, April 13, 2016
4 “The unanswered questions that will impact the success of CPC+”, The Advisory Board Company, April 16, 2016
5 “CMS Announces Major Multi-Payer Comprehensive Primary Care Plus (CPC+) Model”, Health Industry Washington Watch, April 13, 2016
6 Definition obtained from the International Glossary of Business Valuation Terms.





