
Fair Market Value Insights for Multi-Tiered Therapy Service Agreements
Christa Shephard
October 2, 2024
Effective October 8, 2024, Carnahan Group has joined VMG Health. Learn more.
October 15, 2024
Written by Clark Wilson, CVA; Greg Begun; and Ash Midyett, CFA
In the broadest sense, remote monitoring refers to a physician assessing a patient’s health through the use of a medical device or software while physically away from the patient. There are two main types of remote monitoring: remote patient monitoring (RPM) and remote therapeutic monitoring (RTM). RPM focuses on gathering physiological data from medical devices attached to the patient’s body, while RTM focuses on non-physiological data that is generally self-reported.
As it relates to physical therapy, RTM can be used to treat and monitor a wide range of conditions, including musculoskeletal conditions, respiratory conditions, geriatric conditions like osteoporosis, and others. Given the broad range of RTM services, there is a growing list of software providers targeting specific and use cases. Some of these entrants include Medsien, Owlytics Healthcare, and Zimmer Biomet, all of which have proprietary RTM software platforms.
The clinical advantages of RTM include improved adherence to treatment plans, enhanced recovery speeds, reduced re-injury rates, and increased patient satisfaction and engagement. Reducing the chance of reinjury and the number of post-injury visits may increase member satisfaction while enhancing data collection to improve treatment and outcomes. Practices may also see increased patient volumes through improved patient access to care and diagnostics, while minimizing the need for unnecessary in-person appointments.
As a new method of patient engagement, research on the efficacy of RTM remains limited. While research often considers remote monitoring as an effective method of treatment for many conditions, limited research specific to RTM exists for physical therapy applications. Additionally, critics often cite data privacy concerns as a primary headwind for further industry adoption.
In response to the growing adoption of RPM and RTM, the Centers for Medicare & Medicaid Services (CMS) first introduced CPT codes for RPM in 2018 and for RTM in 2021. Since the CPTs were first introduced, CMS has amended billing rules multiple times in response to the pandemic. As of the 2024 Final Rule, CMS allows for billing “incident to” under the direct supervision of a qualified provider (physical therapists, occupational therapists, and speech-language pathologists). RTM and RPM must also be delivered via an approved medical device (which may include software) as certified by the FDA.
The care lifecycle for RTM can generally be characterized by an initial diagnosis, in person or via a telehealth visit, followed by periodic monitoring of the condition, telehealth check ins, or exercise appointments. A provider must monitor a patient for at least 16 days of a 30-day period. As the typical physical therapy course of treatment can range from a few weeks to a couple months, it is easy to understand how RTM may be worked into the treatment life cycle.
RTM is newer than RPM, and payers have been slower to adopt coverage for RTM services as a result. Approved codes are relatively narrow in the scope of conditions covered. Medicaid coverage varies by state, and many states do not have a clear policy around reimbursement. Similarly, commercial payers have been slow to adopt coverage and are generally less likely to cover RTM than RPM.

RTM presents a unique opportunity for physical therapy practices to add an additional revenue stream without significant, up-front investment of time or capital and may broaden the practice’s eligible market for care. With the nearly ubiquitous adoption of mobile phones and growing popularization of fitness wearables, the cost of care for physical therapy RPM and RTM is primarily driven by the cost of software to administer the service ($15–$40 per month) and clinician time.
The RTM industry is in the early stage of the industry lifecycle, characterized by fragmentation, high margins, and a robust growth outlook. Current estimates by the Bipartisan Party Center suggest RPM adoption has been limited but is growing quickly, with 594 monthly claims per 100,000 Medicare enrollees as of 2021, which represents a six-fold increase since 2018. It is too early to say whether RTM will follow a similar growth trajectory. Statistics on usage and efficacy remain limited given the novelty of the technology and the fragmentation of its end market. For instance, there are over 37,000 outpatient rehabilitation clinics in the United States with the largest provider only controlling approximately 5% of the market.
In recent years, the adoption of RPM and RTM has been catalyzed by three primary headwinds: technological progress and the proliferation of mobile devices, an industry-wide shift toward value-based care, and the COVID-19 pandemic. For years, insurance payers, regulators, and thought leaders have heralded the adoption of value-based care initiatives to better align the cost of care with improved patient outcomes. RPM and RTM facilitate data collection and may improve patient outcomes while reducing costs through enhanced recovery speed, improved adherence to treatment plans, reduction in re-injury rates, and improved patient satisfaction and engagement. As value-based care continues to gain market share, RTM technology will likely benefit. The confluence of expanded coverage, patient demand, clinical research, and value-based care advocacy will likely bolster RTM adoption among physical therapy providers. While growth projections remain limited, Global Market Estimates predicts annual RTM market growth in the high teens over the coming years. Physical therapy business operators will likely continue to adopt RTM.
Physical therapy and remote patient monitoring. (2022). Telehealth.HHS.gov. https://telehealth.hhs.gov/providers/best-practice-guides/telehealth-for-physical-therapy/physical-therapy-and-remote-patient-monitoring
Saag, JL & Danila, MI. (2022). Remote Management of Osteoporosis. Curr Treatm Opt Rheumatol. DOI: 10.1007/s40674-022-00195-4. Epub 2022 Sep 2. PMID: 36068838; PMCID: PMC9438367.
ROI of RPM CCM and RTM. (n.d.). Humhealth. https://www.humhealth.com/blog/roi-of-rpm-ccm-and-rtm/
Remote Patient Monitoring (RPM) CPT Code Billing Summary. (n.d.). Healthsnap. https://healthsnap.io/resources/rpm-billing-overview/#:~:text=CPT%20Code%20Billing%20Summary&text=In%202018%2C%20CMS%20began%20providing,reimbursement%20associated%20with%20these%20codes.
Centers for Medicare & Medicaid Services (CMS). (2022). CMS Manual System. CMS. https://www.cms.gov/files/document/r11118cp.pdf
CMS.gov. Calendar Year (CY) 2024 Medicare Physician Fee Schedule Final Rule. (2023). CMS. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-final-rule
Thomas, JJ. (2022). How long is physical therapy session? Primal Physical Therapy. https://primalphysicaltherapy.com/how-long-is-physical-therapy-session/
Curtis, J., et. al. (2024). The Future of Remote Patient Monitoring. Bipartisan Policy Center. https://bipartisanpolicy.org/report/future-of-remote-patient-monitoring/
U.S. Physical Therapy (USPh). (2024). USPh IR Presentation Q1 2024. U.S. Physical Therapy. https://www.usph.com/wp-content/uploads/2024/05/USPH_IR_Presentation_Q1_2024_FINAL.pdf
Global Market Estimates (GME). (2024). Global Remote Therapeutic Monitoring Market Size. Global Market Estimates. https://www.globalmarketestimates.com/market-report/remote-therapeutic-monitoring-market-3954#:~:text=The%20global%20remote%20therapeutic%20monitoring,getting%20infected%20by%20the%20virus
October 10, 2024
Written by Ingrid Aguirre, CFA; Don Barbo, CPA/ABV
A solvency opinion is a professional assessment of a company’s financial health, specifically its ability to meet its long-term obligations. This opinion evaluates whether a company is solvent—meaning its assets exceed its liabilities—based on both current and projected financial conditions and that it has the ability to pay its obligations within a specified amount of time if required by lenders. A solvency opinion serves as a critical tool in corporate finance and transactional contexts, providing stakeholders with confidence in a company’s financial viability.
Solvency opinions are vital for ensuring compliance with various legal and regulatory requirements. They assure boards of directors, shareholders, and lenders that financial decisions—such as mergers, acquisitions, and dividend distributions—are made with a clear understanding of the company’s financial standing.
By obtaining a solvency opinion, companies can mitigate risks associated with potential insolvency claims. A well-supported opinion can protect directors and officers from liability by demonstrating that they acted in good faith and made informed decisions based on sound financial analysis.
A credible solvency opinion enhances transparency and builds trust among investors, creditors, and other stakeholders. It reassures them that the company is on solid financial footing, thereby facilitating smoother transactions and negotiations.
In a litigation context, solvency opinions play a pivotal role.
If a company faces lawsuits related to insolvency, such as fraudulent transfer claims, an independent solvency opinion can serve as a robust defense. It provides evidence that the company was solvent at the time of the transaction in question, helping to protect against accusations of misconduct.
Solvency experts can be called to provide testimony in court, explaining the methodologies and analyses that led to the solvency opinion. Their insights can clarify complex financial matters for judges and juries, lending credibility to the company’s position.
In disputes involving insolvency, a well-prepared solvency opinion can facilitate settlement discussions. It provides a factual basis for negotiations, helping to establish fair terms based on the company’s actual financial situation.
VMG Health provides comprehensive solvency opinions tailored to your specific needs. Our team of financial experts uses rigorous analysis and proven methodologies to ensure our opinions stand up to scrutiny, both in and out of the courtroom.
Our services include:
Secure your company’s financial future and protect your interests with a reliable solvency opinion from VMG Health. Contact us today and discover how we can help you navigate the complexities of financial integrity and legal compliance.
Hayes, A. (2024). What Is Solvency? Definition, How It Works With Solvency Ratios. Investopedia. https://www.investopedia.com/terms/s/solvency.asp
Jacobsen, C. (2018). Solvency Opinions: Legal Insights and Best Practices for Valuation. BV Research Pro. https://www.bvresources.com/articles/training-event-transcripts/solvency-opinions-legal-insights-best-practices-for-valuation
Jacobson, C. A., & Selbst, S. B. (2014, July 9). BVR’s Advanced Webinar Series on Valuations for Business Transactions: Part 1: Solvency Opinions [Webinar]. Business Valuation Resources LLC.
May 2, 2024
At VMG Health, we’re dedicated to sharing our knowledge. Our experts present at in-person conferences and virtual webinars to bring you the latest compliance, strategy, and transaction insight. Sit down with our in-house experts in this blog series, where we unpack the five key takeaways from our latest speaking engagements.
I spoke with King and Spalding attorney Kim Roeder on different, hot-button issues that arise when structuring and valuing different value-based arrangements. It started off as a presentation of different case studies and focused on what Roeder has encountered from a legal perspective and what I have encountered from a valuation perspective. We often receive questions when it comes to structure or even value drivers, and we wanted to present solutions to what we saw or clients struggling with so that they could develop a better understanding of them.
The focus on the metrics themselves and how carefully they need to be considered seemed to be the most surprising. Recent regulations have been really focused on metrics, and that’s what we get the most questions about. I think our audience was also surprised to learn that Kim had experienced those questions as well, and metrics aren’t just a consideration on the valuation perspective. Both legal and valuation perspectives must carefully consider metrics.
Our presentation was a very pragmatic way of illustrating six key issues that often come up during valuation. It’s a great resource for healthcare leaders to reference as they go through and check the boxes to ensure they have thought through all of the considerations that we often see as eleventh-hour issues.
I co-wrote a section of the 2023 Physician Alignment: Tips and Trends Report that discusses quality incentives for providers. It captures key factors to consider, from a valuation perspective, when looking to enter value-based arrangements and where to start.
Value-based arrangements require a very orchestrated balance between legal and compliance, operational champions, and valuation teams. Operational teams should be able to focus on what changes and improvements they want to implement, valuation teams must have an understanding of those goals, and legal and compliance must be involved to ensure the approach is appropriate and compliant. Without cohesion between these three groups, we see those eleventh-hour issues pop up.
Our team serves as the single source for your valuation, strategic, and compliance needs. If you would like to learn more about VMG Health, get in touch with our experts, subscribe to our newsletter, and follow us on LinkedIn.
September 5, 2023
By Sydney Richards, CVA, Patrick Speights, and Christopher Tracanna
Approximately 45.0% of acute care discharges are subsequently admitted to a post-acute setting nationwide, including approximately 4.0% who are admitted to an inpatient rehabilitation facility (IRF). An IRF is a freestanding inpatient facility or specialized unit within an acute care hospital that offers intensive rehabilitation to patients after illness, injury, or surgery. Now more than ever, investment demand for IRFs is strong due to the unique value propositions relative to other healthcare verticals, including strong clinical outcomes at an efficient price to payors, a period of stable regulations, rising patient demand, and a high margin for efficient operators.
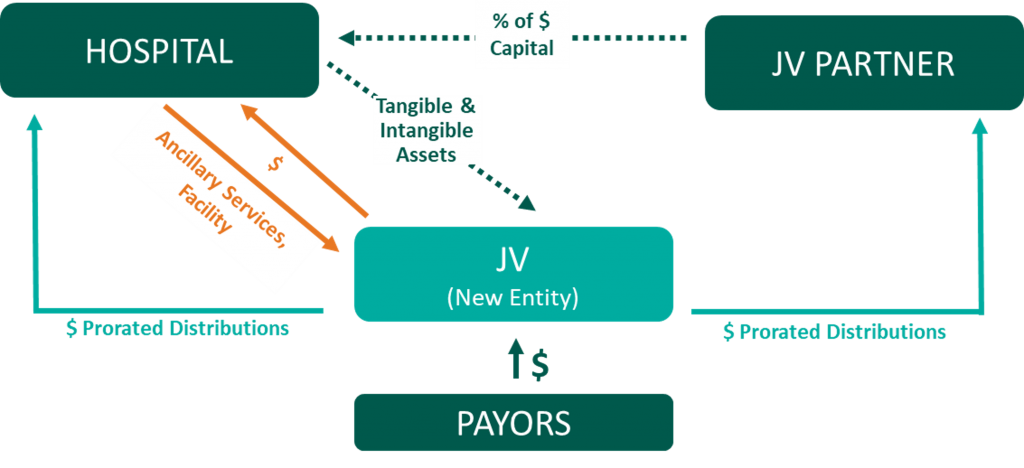
In response to this demand and the potential for high returns, acute care operators may consider affiliating their existing inpatient rehabilitation units (IRUs) with platform post-acute operators to drive financial returns while improving patient outcomes. IRUs are operated as distinct departments of acute care hospitals, while IRFs are freestanding facilities. Going forward we will use the generic term IRF when discussing the inpatient rehabilitation industry.
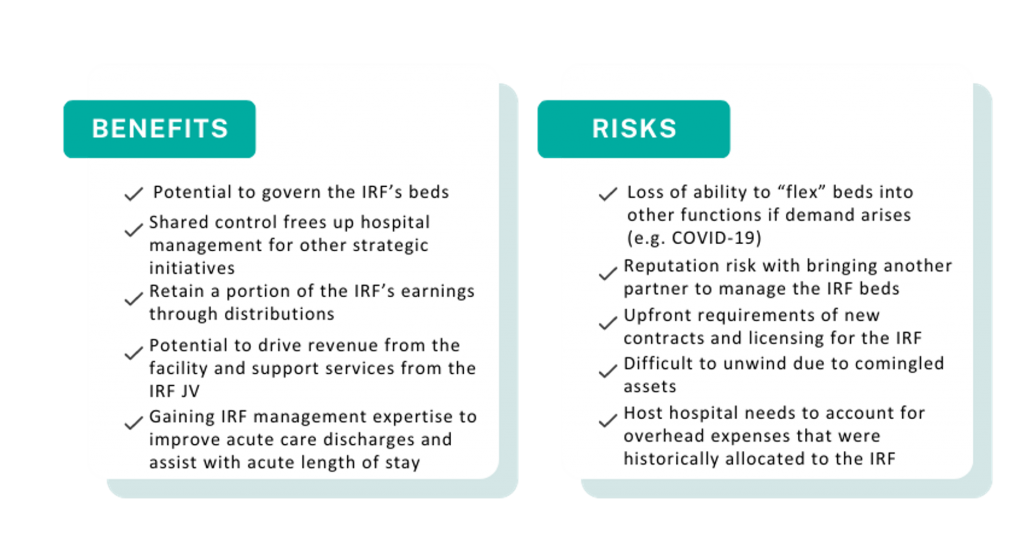
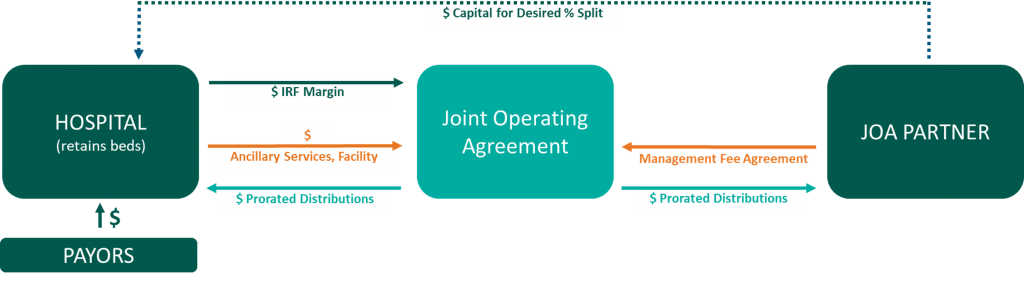
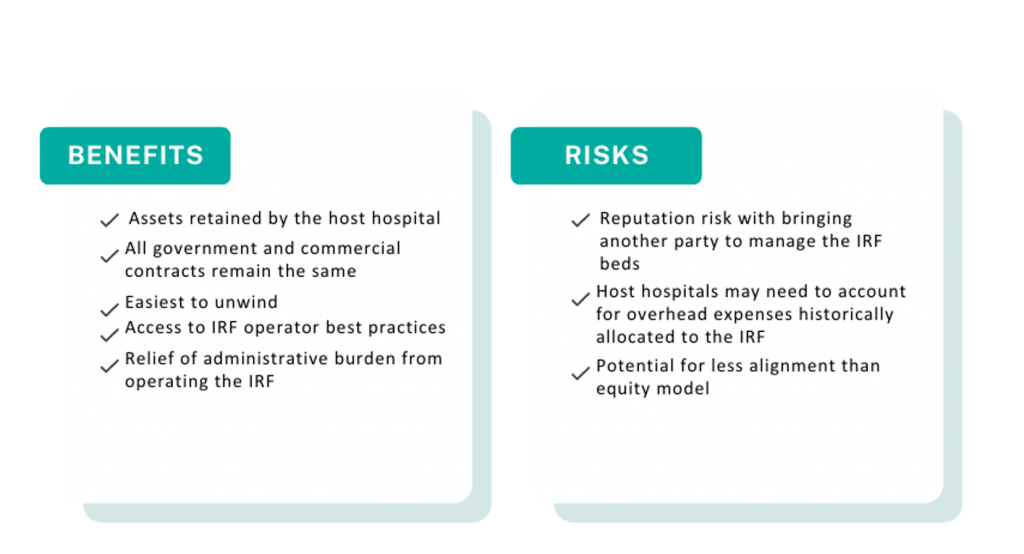
Below, VMG Health experts highlight key industry facts driving up investment. Additionally, our experts detail the potential benefits and risks of common IRF affiliation models, such as joint ventures, joint operating agreements, divestitures, and management agreements.
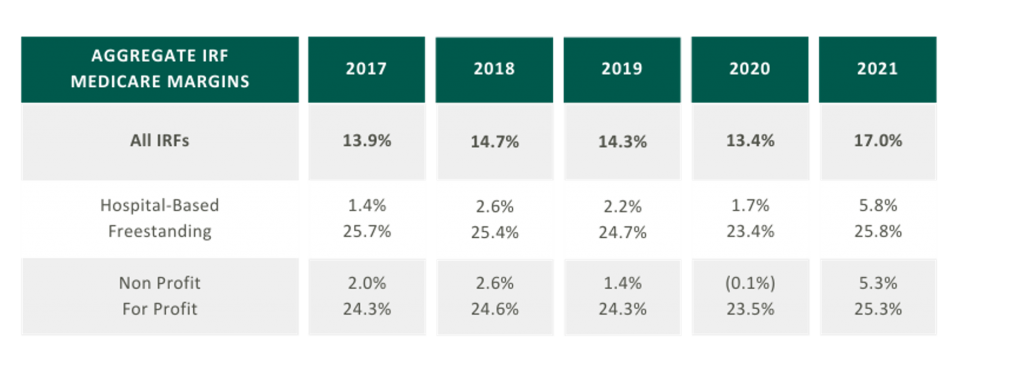
As presented in the table in the below, aggregated IRF Medicare margins were at a five-year high in 2021 at 17.0%. One driver of this increase is the Centers for Medicare and Medicaid Services (CMS) COVID-19 waivers that allowed flexibility in admission criteria and therapy requirements to maintain IRF status. Now that the emergency declaration has ended, margins may become more pressured as IRFs return to standard operating criteria. It is also notable that freestanding Medicare margins were 25.8% in 2021 compared to hospital-based margins of 5.8%. Many factors contribute to this difference, including:
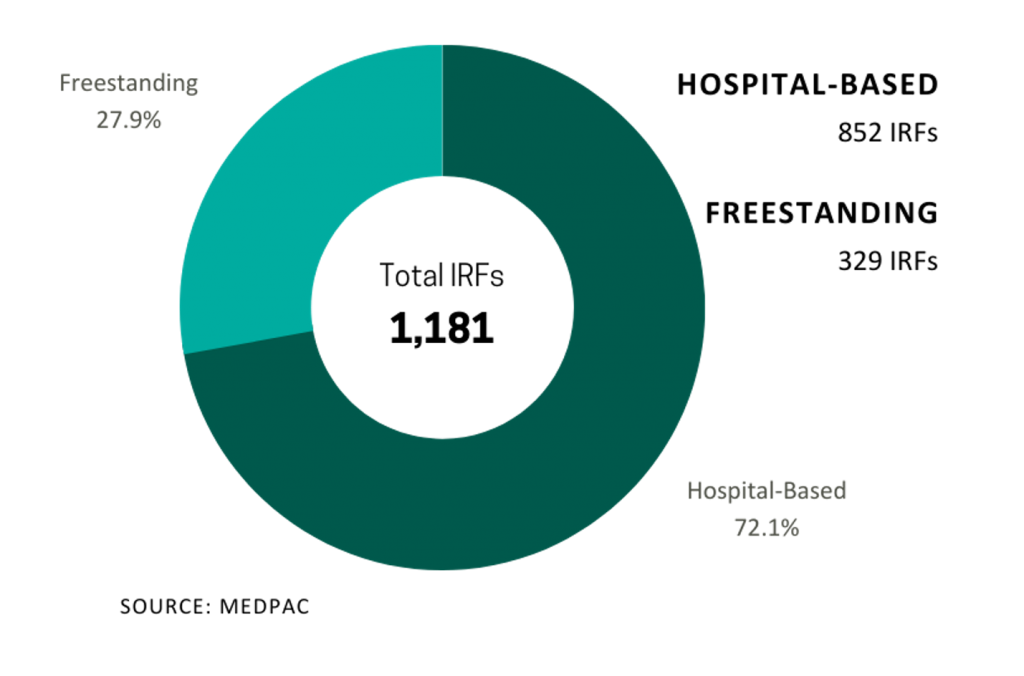
In 2021, five IRFs closed while 22 new IRFs began operations, resulting in a net gain of 17 IRFs. According to MedPAC, the majority of new IRFs were freestanding and for-profit, and most closures were hospital-based nonprofits. As reflected in the chart on the right the top six freestanding IRF operators control approximately 91.5% of freestanding IRFs in the market.

In 2021, Medicare spent $8.5 billion on 379,000 fee-for-service (FFS) discharges across 1,180 IRFs nationwide. These FFS Medicare stays accounted for approximately 52.0% of IRF discharges on average.
Despite the proliferation of specialized post-acute IRF operators, the IRF industry remains fragmented with over 70.0% of all IRF locations being hospital-based IRUs. The remainder are freestanding facilities. However, based on their relatively larger size and bed counts, freestanding IRFs accounted for approximately 55.0% of Medicare discharges. Additionally, while for-profit IRFs make up about 37.0% of all IRFs, they account for approximately 60.0% of the total Medicare discharges.
Many of the aforementioned factors turned the IRF industry into an attractive sector for a strategic post-acute investor. For acute care systems, collaborating with a post-acute operator can offer significant benefits, including reducing the length of stay and readmission rates, and providing access to clinical and operational best practices. Collectively, these enhancements improve both patient outcomes and financial returns. We have identified several affiliation models for post-acute and IRF unit operators, as well as advantages and disadvantages to consider for each model.



A post-acute care strategy is vital for acute care providers seeking to elevate patient outcomes while maximizing value to their organization. Forming strategic alliances with post-acute operators in inpatient rehabilitation may be one successful approach. Operators have many avenues to consider whether it is through the sale of an existing inpatient rehabilitation unit, joint venturing with a partner to create a de novo freestanding IRF, or employing a post-acute manager to drive performance in an existing IRF. No matter your path forward, VMG Health experts can provide actionable insights into the value of your existing IRF business and assist with a potential IRF partnership in a model that fits your post-acute strategy.
Sources
December 15, 2022
By: Madi Whyde, Savanna Ganyard, CFA, Jordan Tussy, and Madison Higgins
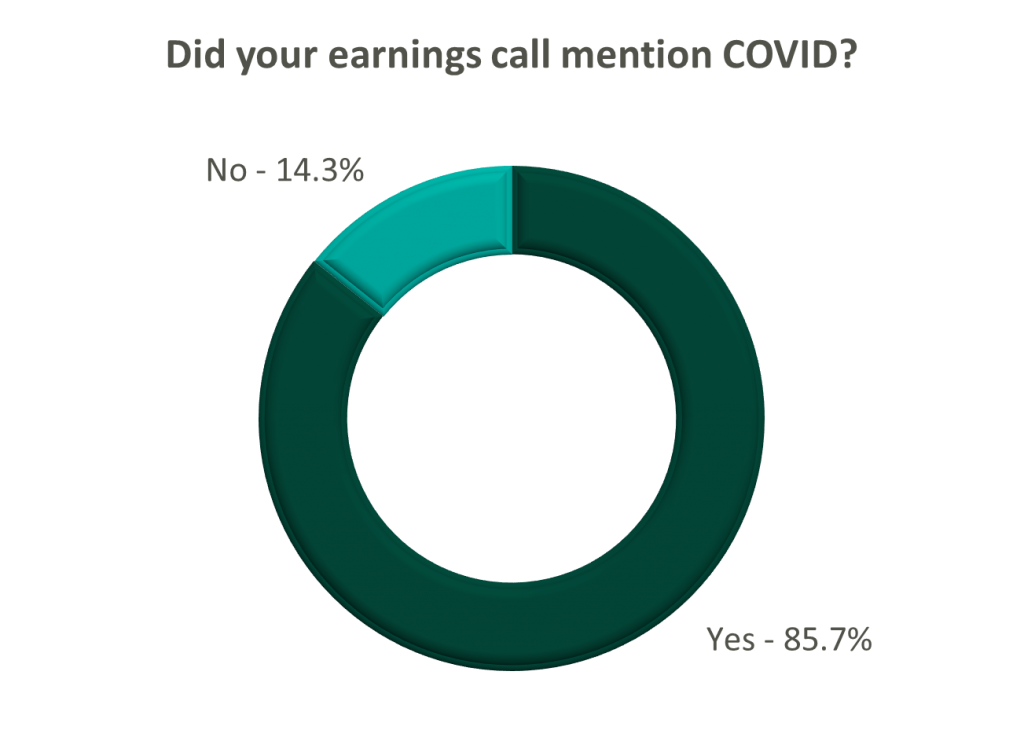
VMG Health reviewed the earnings calls of publicly traded healthcare operators that reported earnings for the third quarter that ended on September 30, 2022. By focusing on the major players in select subsectors defined below, we analyzed the frequency of certain keywords including inflation, COVID-19, interest rates, premium labor, and others. We used these keywords to identify which topics commanded the room this earnings season. Highlights from the calls are summarized in this article.
Volume: Although volume trends are unique to each industry sector nearly all operators remained focused on the impacts of COVID.
Poll: Did the earnings call mention COVID-19?
On a same-facility basis, admission volumes declined as much as 5.0% from the comparable prior year quarter (Q3 2021) for acute care hospital operators. Despite the weakening of COVID-19, the decline in volumes was attributed to higher-than-average cancellation rates (THC), the migration of certain procedures to outpatient status (CYH and HCA), and capacity constraints (HCA). Inpatient volumes generally remained at or below pre-pandemic levels.
Ambulatory surgery center (ASC) operators reaped the benefits of the migration to the outpatient setting and reported positive volume trends when compared to Q3 2021. Surgical volumes were reported as consistent with 2019 pre-pandemic levels (THC), and one operator claimed the business did not experience any material direct impact related to COVID-19 during Q3 2022 (SGRY).
The post-acute sector reported mixed results in volume trends. One operator reported a year-over-year decline of 14.0% in hospice admissions, citing capacity constraints and reduced referrals from acute care hospitals (EHAB). However, another operator indicated that increases in admissions in the second half of the third quarter showed growth that they “haven’t experienced since the start of the pandemic” (CHE).
Volume trends among other industry players including dialysis providers, risk-bearing organizations, and physician services were also affected by COVID-19 in Q3 2022. Headwinds in dialysis volumes are expected to persist for the foreseeable future (DVA), and inpatient volumes for risk-bearing organizations remain below pre-pandemic levels (AGL). Notably, AGL also reported a rebound in physician office visits and outpatient volumes were in line with pre-pandemic levels.
Reimbursement: Declining COVID-19 volumes mean less incremental government revenue for certain industry players who also now contend with an uncertain inflationary environment.
Poll: Did the earnings call mention inflation?
Declining COVID-19 volumes resulted in lower acuity patients and reduced incremental government reimbursement. This softened the reimbursement per admission for the acute care hospital segment. Further exacerbated by inflation, these dynamics were evident in reported EBITDA margins which declined as much as 17.0% (CYH) over Q3 2021. In response, some acute care hospital operators are turning to commercial payor negotiations. Rate increases for the next year are anticipated to range from a minimum of 3.0% (THC) to upwards of 6.0% (CYH).
The post-acute sector did not release specific figures regarding contract rate hikes. However, the sector is optimistically looking for high single-digit rate increases (SEM) to provide relief in the current inflationary environment.
Labor: Unsurprisingly, management teams across the sector were faced with questions about labor trends and management techniques during their earnings calls. Contract labor remained pivotal for the operations of some, but premium labor appears to have softened during the quarter.
Poll: Did the earnings call mention premium or contract labor?
The reliance on contract labor continued its downward trend in Q3 helping moderate expenses. HCA even indicated overall labor costs were stable due to targeted market adjustments. However, contract labor and premium pay remain at uncomfortably high levels for most acute care hospital operators. UHS revealed during their call it will be unlikely to reach pre-pandemic levels in the near future.
Staffing challenges persisted among the post-acute operators and directly impacted volume by as much as 60.0% (AMED). Increased indirect labor costs including orientation, training, and sign-on bonuses were the leading drivers of decreased EBITDA (AMED). Wage inflation, particularly for nursing positions, is expected to rise as much as 5.0% next year (SEM). However, several management teams are optimistic wages will stabilize to historical levels (SEM, EHC) in the near future.
Other industry players, including dialysis and physical therapy providers, also faced challenges with contract labor during the quarter. USPH reported labor costs were approximately 200 basis points higher than Q3 2021 levels, and DVA indicated such costs showed no improvement.
Go Forward Expectations and Guidance: Considering the quarter’s performance, the companies we reviewed were divided relatively evenly in terms of revised FY 2022 revenue guidance, (i.e., raised, lowered, unchanged). In general, the quarter brought about a more pessimistic view of FY 2022 EBITDA, and the majority of public companies lowered their guidance for the year. Further, most stakeholders were left with no guidance for FY 2023.
Poll: Did the earnings call mention a recession?
FY 2022 revenue and EBITDA guidance among the acute care hospital operators was generally left unchanged except for THC which lowered EBITDA guidance. However, all companies that were reviewed declined to provide FY 2023 guidance during the call, and primarily cited economic uncertainty (HCA).
The post-acute sector appeared nearly unanimous in the outlook for the rest of 2022, and most operators lowered their revenue and EBITDA guidance. Unsurprisingly, no one offered FY 2023 guidance during the earnings calls.
Interestingly, risk-bearing organizations mostly raised their revenue guidance for FY 2022 (AGL, CMAX, PRVA). However, EBITDA guidance was less predictable and was lowered (AGL, TOI), raised (PRVA), and unchanged (CMAX).
Most other healthcare operators followed similar patterns in terms of providing guidance for FY 2023. Of the companies we reviewed, only DVA revealed an outlook for the next year. The company anticipates revenue to be flat (driven by unfavorable volume trends) and margins to continue to feel the impact of labor market pressures.
June 27, 2022
Inpatient rehabilitation utilization has experienced remarkable growth over the past decade, fueled by a demographic boom in the industry’s primary patient population, stable regulations, and continued Medicare reimbursement increases. Per the 2022 MedPac Report [1], inpatient rehabilitation facilities (IRFs) accounted for $8 billion of Medicare spending in 2020, and paid out to about 1,160 IRFs and inpatient rehabilitation units (IRUs) nationwide. IRUs are operated as distinct part units of an acute hospital compared to an IRF which is a licensed freestanding facility.
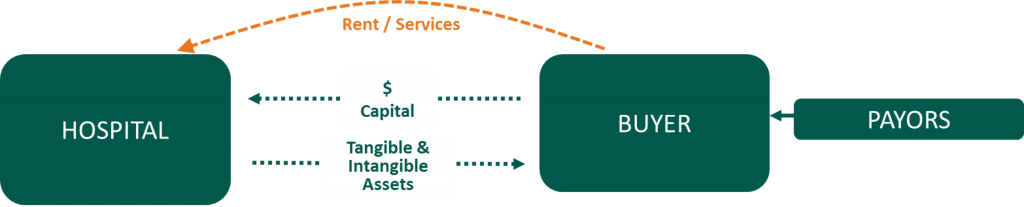
As the Medicare population continues to grow [2], and industry data increasingly demonstrates both the clinical efficiency and cost-effectiveness [3] of inpatient rehabilitation compared to alternative post-acute alternatives, inpatient rehabilitation utilization is expected to continue to climb. Additionally, with the low cost of capital and proliferation of strategic post-acute buyers available, it is a seller’s market for IRFs. These trends are causing many acute care operators to question whether they should monetize their hospital based IRU by selling or partnering with a third party.
Selling or partnering an IRU can provide numerous benefits to an acute care provider, including the following:
The healthcare provider market saw a decrease in the number of transactions in 2020 due to the global pandemic, but according to Irving Levin’s 4th Quarter 2020 M&A report [4] Q4 2020 saw a dramatic recovery in both healthcare deal volume and spending. [3] Based on VMG Health’s 20-year IRF-specific transaction database, IRF average values per occupied bed are trending at a 10-year high. Favorable returns for sellers and buyers are fueling this growth. Post-acute management companies such as Encompass Corp., Kindred Healthcare, and Select Medical have made public their IRF-focused growth objectives and their demand for strategic partnerships with IRFs in markets across the US.
In their September 2020 presentation at the Baird 2020 Global Healthcare Conference, Encompass CEO Mark Tarr reiterated Encompass’s aim to add 100 to 150 beds per year starting in 2021 through de novos and acquisitions. [5] Kindred also stated in a December 1, 2020 press release that they expect “to open 20 new rehabilitation hospitals, acute rehabilitation units, and behavioral health hospitals with leading strategic hospital partners over the next two years.” [6] These factors suggest an opportunity for acute care providers to capitalize on their rehabilitation units through a sale or joint venture model.
Through a sale or partnership, the acute care provider can drive operational excellence for the host hospital by generating additional bed capacity within the health system and potentially lowering the hospital’s average length of stay. An IRF management company with access to best practices in patient admission criteria and IRF regulatory rules could allow for quick patient assessment and discharge from an acute setting to an inpatient rehabilitation facility. If bed capacity or length of stay are not issues for the host hospital, a partnership with a management company could provide additional revenue from facility lease arrangements and patient service contracts. Also, if market demand is present for additional IRF beds, the IRF partnership could use additional nonoperational beds from the host hospital to provide income from otherwise nonprofitable hospital space. Finally, the partnership could license the host hospital’s tradename as another opportunity to capitalize on an existing asset for revenue or joint venture equity.
In addition to driving operational excellence for the host hospital, a sale or partnership with a strategic buyer can advance the IRF’s top-notch quality care and clinical effectiveness at efficient costs. Using knowledge of clinical best practices, therapy recruiting and training, and economies of scale, strategic post-acute providers can drive high-quality care at a more profitable rate and obtain additional returns for the hospital partner. MedPac data corroborates this claim with for-profit aggregate IRF Medicare margins at 24.2% of revenue as compared to nonprofit margins at just 1.5% (see table below).

Additionally, a sale or partnership can insulate an acute care provider from future regulatory burdens or risks. Historically, the inpatient rehabilitation industry has dealt with material legislative changes to patient admissions and quality reporting standards. Specialized post-acute care providers can navigate industry requirements like the Centers for Medicare & Medicaid Service (“CMS”) 60% Rule [7] and the three-hour therapy care rule [8] while providing additional patient access and quality patient care.
As new developments arise, such as continual revisions to the CMS Inpatient Rehabilitation Quality Reporting Program and patient admission criteria, inpatient rehabilitation-specific operators have the concentration and corporate strategy teams in place to study new legislation and its potential impact on operations. Additionally, a sale or partnership can provide a health system with some protection against future reimbursement risks in the industry. MedPac’s annual report to Congress has suggested a 5.0% reduction in the Medicare reimbursement rates for inpatient rehabilitation reimbursement every year from 2017 to the latest report published in March 2022.1 This was in response to the climbing aggregate Medicare margins in the industry, which in 2020 were 13.5% across all IRFs (freestanding and hospital-based, excluding Medicare COVID relief funds), according to the 2022 MedPac report. [1] MedPac estimates the 2020 aggregate Medicare margin was 14.9% including estimated Medicare share of federal relief funds. Although CMS has continued to project positive reimbursement growth in the final rule, if margins continue to rise it is expected that reimbursement may eventually be reduced. Based on the 2020 -0.7% aggregate Medicare margin for nonprofits (2.6% inclusive of federal relief funds) and the 1.6% aggregate Medicare margin for hospital-based IRFs (4.0% inclusive of federal relief funds), it is unlikely that a 5% Medicare reimbursement cut would be viable for many hospital-based IRFs in these settings.
Finally, the sale or partnership of a rehabilitation unit allows the hospital to continue its integrated delivery model with a partner in post-acute care or have a partner ready to implement an integrated network. As CMS transitions to value-based payments and outcome focus, aligning with or selling to a strategic partner could provide the hospital with focused expertise in managing patient readmission. Multiple management companies, such as Encompass, Kindred, and Select, have proven success with risk-sharing models with acute care providers. This could help the health system with both care quality and profitability.
Although there can be many benefits to selling or partnering an IRU, as with any business transaction, there are also some drawbacks. For an acute care provider, a key downside can be the loss of control. The acute care provider would lose the ability to flex its bed use if the inpatient rehabilitation beds were sold or contributed to a joint venture. The ability to flex beds became an important capability during the COVID-19 outbreak in the US. Additionally, under a joint venture partnership, the acute care provider opens itself up to reputation risk since control and management of the IRU is entrusted to a third party. Through a sale or partnership, the acute care provider sells forward profits, and the host hospital needs to account for the overhead expenses that were historically allocated to the IRU.
In summary, many acute care providers should ask, “Are they generating the most value from their IRU as they could or should?” A sale or partnership of the IRF could add value to the health system beyond the initial cash flow from a transaction. The relationship between an acute care host hospital and the IRF is considered a referral relationship with Medicare patients. Therefore, whether through a sale or contribution, healthcare transactions must be properly established at fair market value. Based on VMG Health’s experience with hundreds of IRF transactions, the departmental operational reports never represent IRF’s real economic impact on the host hospital. As many IRUs operate as departments of hospitals and utilize allocated cost methodologies, it can be a highly technical undertaking to assess the profitability and overall value of an IRU. Specific knowledge and insight into key industry value drivers, such as reimbursement/payor mix, staffing metrics, unit size/bed configuration, and utilization, should be considered. A credible valuation with access to a detailed national IRF benchmark analysis9 for revenue and expenses can help ensure a successful transaction.
To provide some IRF value perspective, VMG Health has observed IRF transactions per occupied bed as high as $800,000, with common value ranges per licensed bed between $200,000 and $400,000, and revenue multiples typically falling in the 0.8–1.4x range. This year might be a great time to ask, “Is your IRU generating the value your patients have come to expect, supporting your healthcare strategy, and adding value to your bottom line?”
[1] MedPac 2022 Report (https://www.medpac.gov/wp-content/uploads/2022/03/Mar22_MedPAC_ReportToCongress_Ch9_SEC.pdf
[2] Medicare population projected at 5% annually over the next several years.
[3] Census projections for 2018 to 2022 and 2022 to 2026. https://www.census.gov/data/datasets/2017/demo/popproj/2017-popproj.html
[4] Encompass Health Investor Reference Book https://s22.q4cdn.com/748396774/files/doc_downloads/investor_reference/2020/11/EHC-Q3-2020-Investor-Reference-Book_11-13-20_As-Filed.pdf
[5] Irvin Levin’s 4th Quarter 2020 M&A Report
[6] Baird 2020 Global Healthcare Conference https://investor.encompasshealth.com/events-and-presentations/other-events-and-presentations/event-details/2020/Baird-2020-Global-Healthcare-Conference/default.aspx
[7] Kindred Healthcare December 1, 2020 Press Release (https://www.kindredhealthcare.com/about-us/news/2020/12/01/kindred-healthcare-advances-growth-strategy-completes-sale-of-rehabcare
[8] Medicare reimbursement per episode of care for inpatient rehabilitation is generally higher as compared to other post-acute facilities because IRFs are designed to offer intensive rehabilitation services to patients that cannot be served in other less intensive rehabilitation settings, such as skilled nursing facilities or home health. Due to the higher reimbursement, CMS became concerned that patients who did not require intensive rehabilitation services were being treated in an IRF setting. Therefore, CMS implemented the 75% rule which required that 75% of patients admitted to an IRF have a primary diagnosis or comorbidity in one of the 13 qualifying medical conditions listed in the table below. After implementing, Medicare adjusted the 75% rule to a new compliance threshold of 60% by the Medicare, Medicaid, and SCHIP Extension Act of 2007 (“MMSEA”). In addition, MMSEA also permitted IRFs to use patient’s secondary medical conditions & comorbidities to determine whether a patient qualifies for inpatient rehabilitative care. The legislation is referred to as the “60% Rule.”
[9] In addition to the 60% rule, to be eligible for payment as an IRF under CMS, patients must attend three hours of therapy in 5 of 7 consecutive days.
[10] VMG Health’s proprietary inpatient rehabilitation database includes 20 years of inpatient rehabilitation analyses with over 100 IRF transactions.
February 9, 2022
As we enter 2022, we look back to reflect on the major trends that shaped the healthcare sector over the past year. COVID-19 continued to be a major player throughout 2021, forcing healthcare systems to adapt to new variants, rising labor pressures, financial activity, and new regulations. Despite these challenges, the sector remains optimistic and ready to adapt.
Here are five key takeaways we believe defined the healthcare sector over the past year:
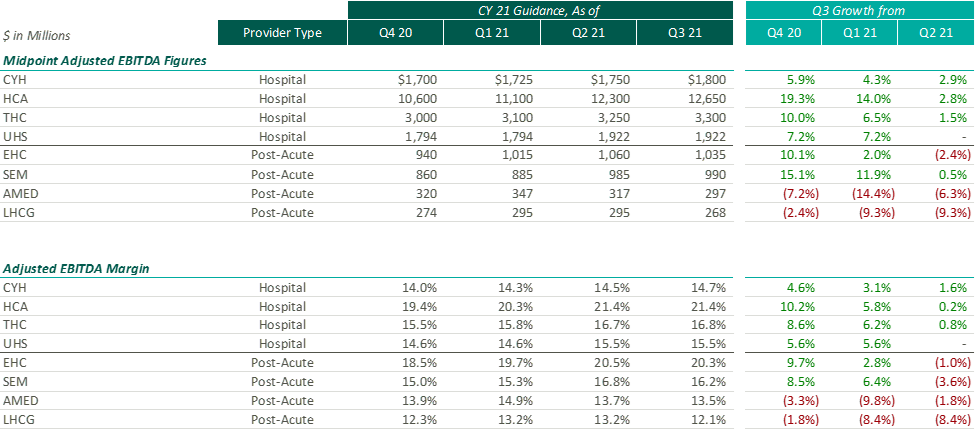
After the Q2 earnings season, VMG Health released an article analyzing post-COVID healthcare operator guidance. Generally, we found that healthcare operators were optimistic about the recovery of their revenue and adjusted EBITDA metrics over pre-pandemic levels, with most operators increasing their FY 2021 guidance with each subsequent reporting period.
While optimism for recovery to pre-pandemic levels remains, it appears that the post-acute operators have tempered some of their recent growth expectations. Based on disclosures of the public operators, the recent resurgence of COVID-19 through the Omicron variant has caused additional strain on the post-acute sector. During the J.P. Morgan Healthcare Conference, Universal Health Services (“UHS”) CFO, Steve Filton noted that the company was struggling to find providers who can accept COVID patients once they are ready to be discharged from the hospital.
Post-acute providers appear to have been hit especially hard by the recent labor shortages in the healthcare industry (discussed further below). As compared to the hospital operators, the financial performance of these post-acute providers has been affected disproportionally by the labor shortages. While hospital operators have been receiving additional reimbursement for COVID patients, helping to offset a portion of the increased staffing costs, the post-acute care providers have not received a similar subsidy.
Due to these recent pressures, Select Medical Holdings Corporation (“SEM”) released an expected earnings announcement in advance of the actual results, in which it noted “the unpredictable effects of the COVID-19 pandemic, including the duration and extent of disruption on Select Medical’s operations and increases to our labor costs, creates uncertainties about Select Medical’s future operating results and financial condition.”
While we have seen increasing optimism by healthcare providers over the past few quarters, the recent disclosures from the post-acute sector illustrate that the effects of COVID continue to ripple through the healthcare sector. With the fourth quarter results being released over the coming weeks (HCA and Encompass recently released), it will be interesting to hear if other sectors report similar headwinds.
Healthcare labor expenses continued to exceed historical levels with a 12.6% year-over-year increase based on a recent analysis of over 900 hospitals. Labor expenses grew at a faster rate than the number of clinical hours worked, which supports the notion that rising labor costs were not due to increased staffing levels but rather due to labor shortages driving higher pay to improve employee retention. Part of the labor shortage can be credited to the surge of Delta and Omicron variants in the second half of 2021 that resulted in high volumes of quarantined staff and a reliance on costly contract labor and travel nurses. At the Bank of America December 2021 Home Care Conference, LHC Group announced a decrease in quarantined staff throughout Q4 from a high of 4% down to 1% in December. This indicates that the labor market issues will see some improvement as health systems’ dependence on pandemic-related contract labor declines as COVID-19 surges dissipate going into 2022.
A more concerning challenge faced by all sectors was the shrinking workforce, coined the “Great Resignation.” The Bureau of Labor Statistics reported healthcare and social assistance workers had the second highest quit rate in November 2021 at 6.4% due to increasingly high levels of professional burnout. The waning labor force has prompted companies to offer additional incentives such as shift and retention bonuses. For example, HCA reported during Q3 a 10-12% annual increase in FTEs being in the premium pay categories. Many large public players have voiced an anticipation of continued high levels of premium pay, competitive bases, and higher annual wage inflation to attract and maintain adequate staffing levels in 2022.
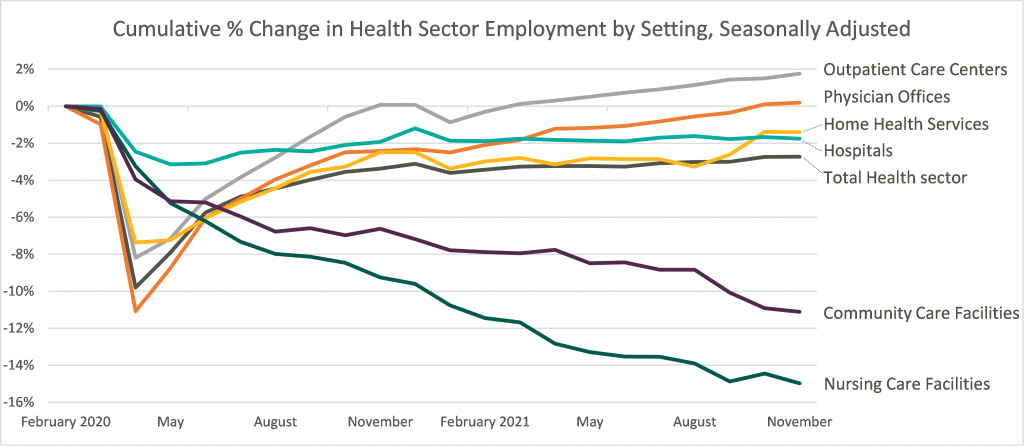
Leaders in the industry have announced initiatives to decrease labor pressure primarily by focusing on recruiting and retention to bounce back to pre-pandemic levels of employment. With a heightened focus on attracting and maintaining adequate levels of hired staff as opposed to contract labor, it appears the overall industry expectation for 2022 is that labor costs will likely decrease compared to 2021 although not to pre-pandemic levels. The chart below shows the percentage change in employment across the healthcare sector from the Bureau of Labor Statistics Job Openings & Labor Turnover Survey from February 2020 to November 2021. This highlights the steady recovery toward pre-pandemic staffing levels for outpatient care and physician offices, the continued employment challenges in home health and hospital settings, and the notable struggle for community and nursing care facilities to return to a state of normalcy.
Deal activity within the healthcare sector was strong in 2021 with industry-specific multiples that reached or in many cases exceeded 2019 levels. Experiencing a noticeable rebound from 2020, volume and value of deals grew by substantial margins on a year-over-year basis. Deal volume in the health services industry rose by 56% while value rose 227% in the TTM 11/15/21 period. Long-term care led all sectors with the highest volume of deals, as seen historically, and continues to remain a hot spot in the transaction space. Similarly, physician medical groups and the rehabilitation sector experienced the largest growth transaction volumes year-over-year.
Physician medical groups have received vast interest in physician employment from private equity firms, new-age value-based care organizations, services arms of managed care giants (Optum, Neue Health), and health systems. This, coupled with independent physician group operating challenges from COVID-19 related volume impact and looming Centers for Medicare and Medicaid Services (CMS) cuts, is creating a robust transaction environment that is expected to continue during 2022. For the rehabilitation sector, strong demographic tailwind, along with the lifted CON moratorium in Florida and continued joint venture interest between health systems and strong rehabilitation operators (Select, Kindred, Encompass), has resulted in material deal volume in the space.
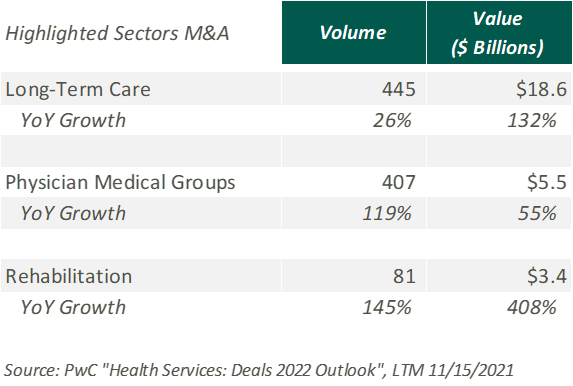
Hospitals and health systems were the only sector to see a decline in volume of deals, down 26% from the previous year. Despite the decline, the total transaction size of deals only dropped slightly year over year, indicating larger deal-size on a per-transaction basis. The acceleration of megadeals taking place, the shifted focus on scale, and the diversification of their business models all drove average total size per deal higher than seen before in 2021.
Effective January 1, 2021, the Centers for Medicare and Medicaid Services (CMS) implemented a price transparency rule requiring hospitals in the United States to provide accessible pricing information to patients about the cost of the care they may receive. Hospitals must display negotiated rates for all items and services, in a machine-readable format, so that patients can compare prices before arriving at the hospital.
Though, in July 2021, a study was published by PatientsRightsAdvocate.org detailing that a vast majority of hospitals were not compliant with the new rule. At the release of the study, the penalty for non-compliant hospitals was $300 per hospital, per day. While many patients advocate for CMS to stiffen penalties for non-compliant hospitals, healthcare professionals argue against the rule, stating CMS did not provide enough clarity on what the rule should entail.
A vice president of a large U.S. health system discussed the ambiguities around the rule with Fierce Healthcare. “One interpretation is you simply publish your rate schedule – whatever your rate exhibits are in your contracts, publish that and that’s compliant. Another one is to summarize these [CMS] packages [and] what your negotiated charges are.” For many health systems, the resources required to implement their rates in a machine-readable format far outweigh the penalty of remaining non-compliant. The VP stated that he believes many hospitals already provide their rates in a clear, understandable way, but the rule’s lack of clarity and the requirement for a machine-readable format make compliance difficult and costly.
In November 2021, CMS released the 2022 Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) Payment System final rule (OPPS Final Rule). Within this rule, CMS increased penalties for hospitals that are not compliant with the price transparency rules and removed barriers for patients accessing online pricing information.
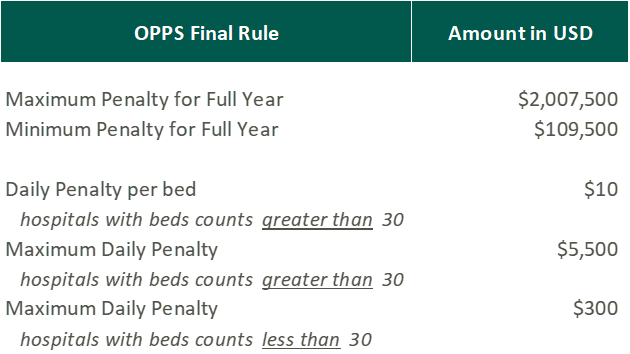
While the Final Rule may be beneficial for patients, Stacey Hughes, Executive Vice President for the American Hospital Association (AHA), states that they “are very concerned about the significant increase in penalties for non-compliance with the hospital price transparency rule, particularly in light of the many demands place on hospitals over the past 18 months, including both responding to COVID-19, as well as preparing to implement additional, overlapping price transparency policies.”
The new penalties, visible in the chart above, went into effect on January 1, 2022.
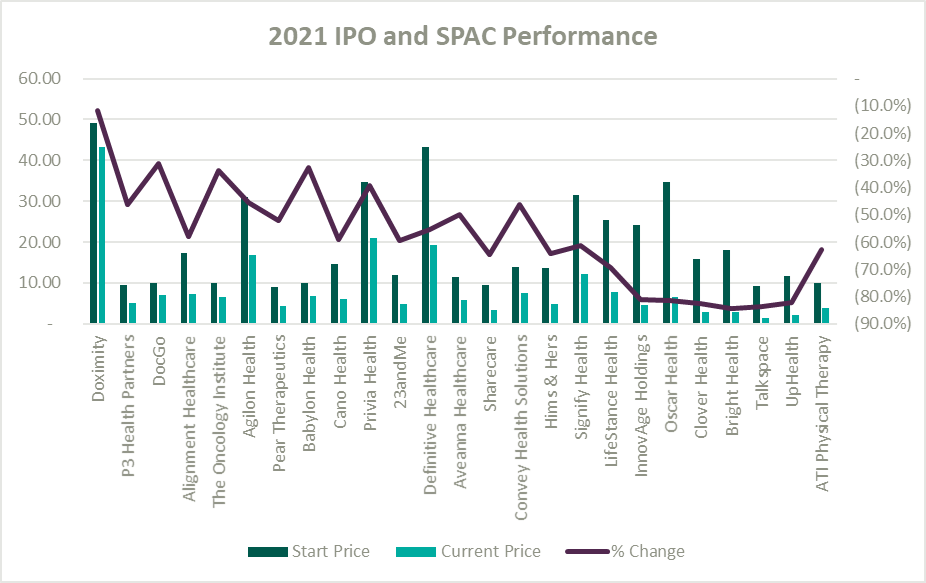
A record number of health and health services companies went public during 2021 by way of SPAC or IPO. Rebecca Springer, a private equity analyst with PitchBook noted, “The multiples in public markets are very, very strong right now, so you can get, all else equal, a better return on your investment if you go public with your company rather than selling it to a strategic investor.”
Unfortunately, while the stock market might be performing well, the recently public healthcare operators have not faired as well since their initial offerings. The Healthy Muse Health Tech Index (“HTI”) generally underperformed the overall performance of the stock market, with the majority of the players finishing in red; the HTI declined 35% as opposed to the 27% gain for the S&P 500 during 2021. The public markets seemed like a perfect place for an exit strategy given the multiples observed in the public markets. All recent entrants finished the year below the original IPO price and while the reasons for the price declines varied it is clear the public markets are less forgiving with valuations if an organization does not achieve expectations.
Overall, the healthcare sector experienced highs and lows during 2021 as it continued to navigate a post-COVID world. As pandemic pressures continue into 2022, healthcare institutions will have to keep a close eye on staffing costs and abide by new regulations. Despite these challenges, the appetite for M&A transactions and market participation in the sector remains strong. We look forward to a new year of challenges, wins, and continued changes in this interesting industry.
https://www.cms.gov/medicare/covid-19/new-covid-19-treatments-add-payment-nctap
https://www.pwc.com/us/en/industries/health-industries/library/health-services-deals-insights.html
https://www.policymed.com/2021/12/cms-announces-increased-fines-for-transparency-violations.html
October 1, 2021
Contributors: Blake Madden, Chris Madden, Alex Malin, Eric Noyer, and Olivia Wilson
In March 2020, the coronavirus (“COVID-19”) pandemic began reshaping the world economy. At the time, many factors about the disease were unknown and impossible to predict. Some of these factors include the evolution of the disease, timeline to produce a vaccine, and the economic effects of worldwide lockdowns. The healthcare industry was uniquely affected, and many healthcare operators felt that they were not in the position to forecast future financial performance. After a year of operations in a COVID-19 impacted world, operators resumed the disclosure of earnings guidance. VMG analyzed guidance figure trends from publicly traded acute care hospitals, post-acute providers, home health and hospice companies, and a variety of other operators to better understand how the industry is recovering and evolving as the pandemic continues.
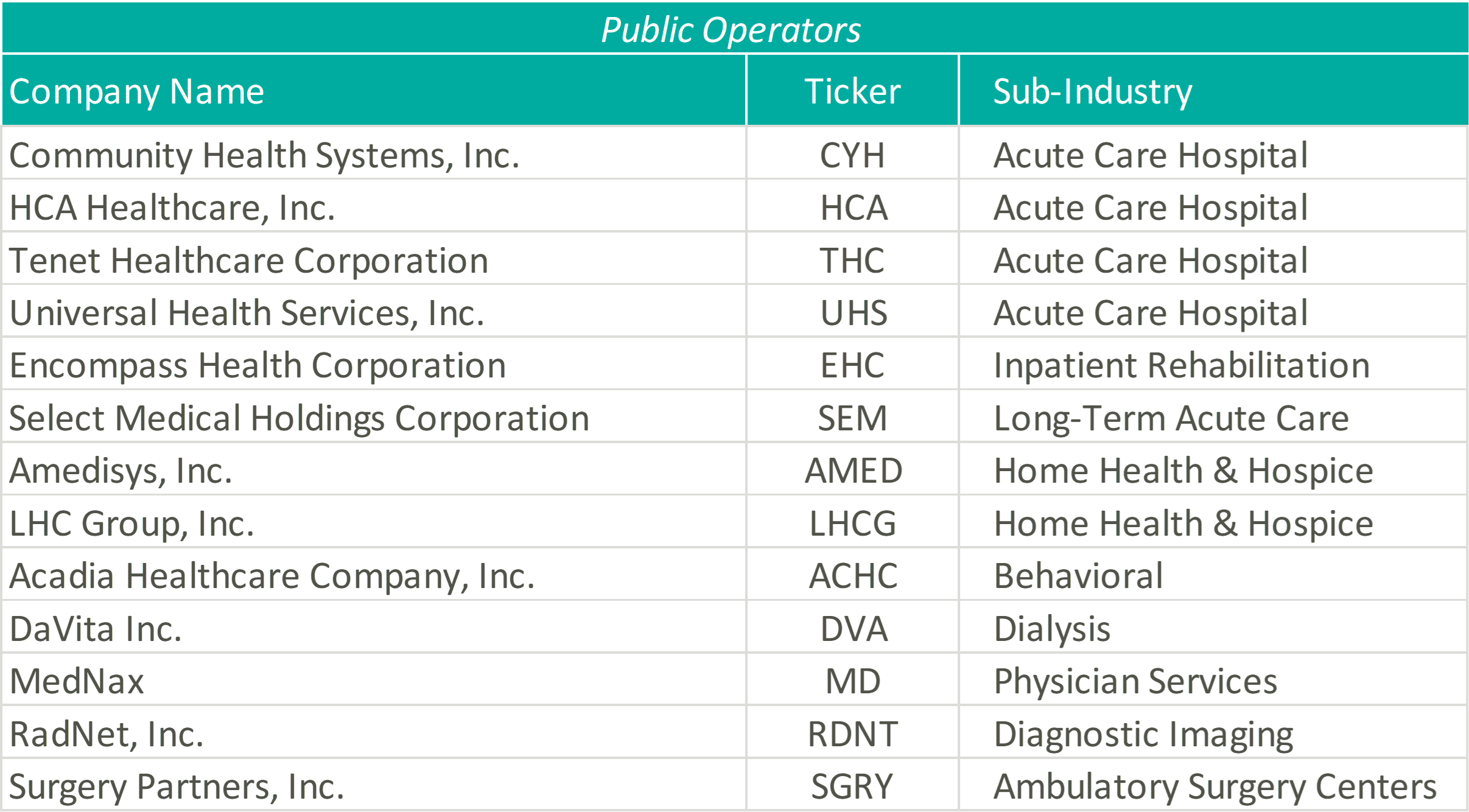
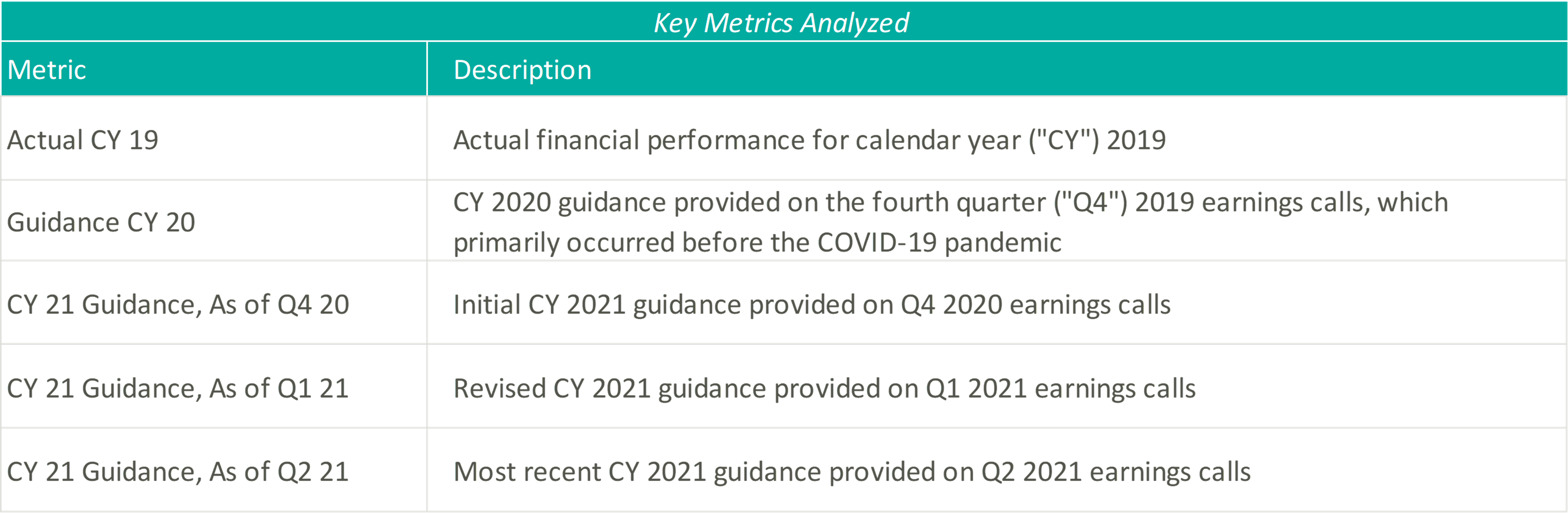
Please see below for a list of the companies examined, as well as further detail regarding the various metrics considered.
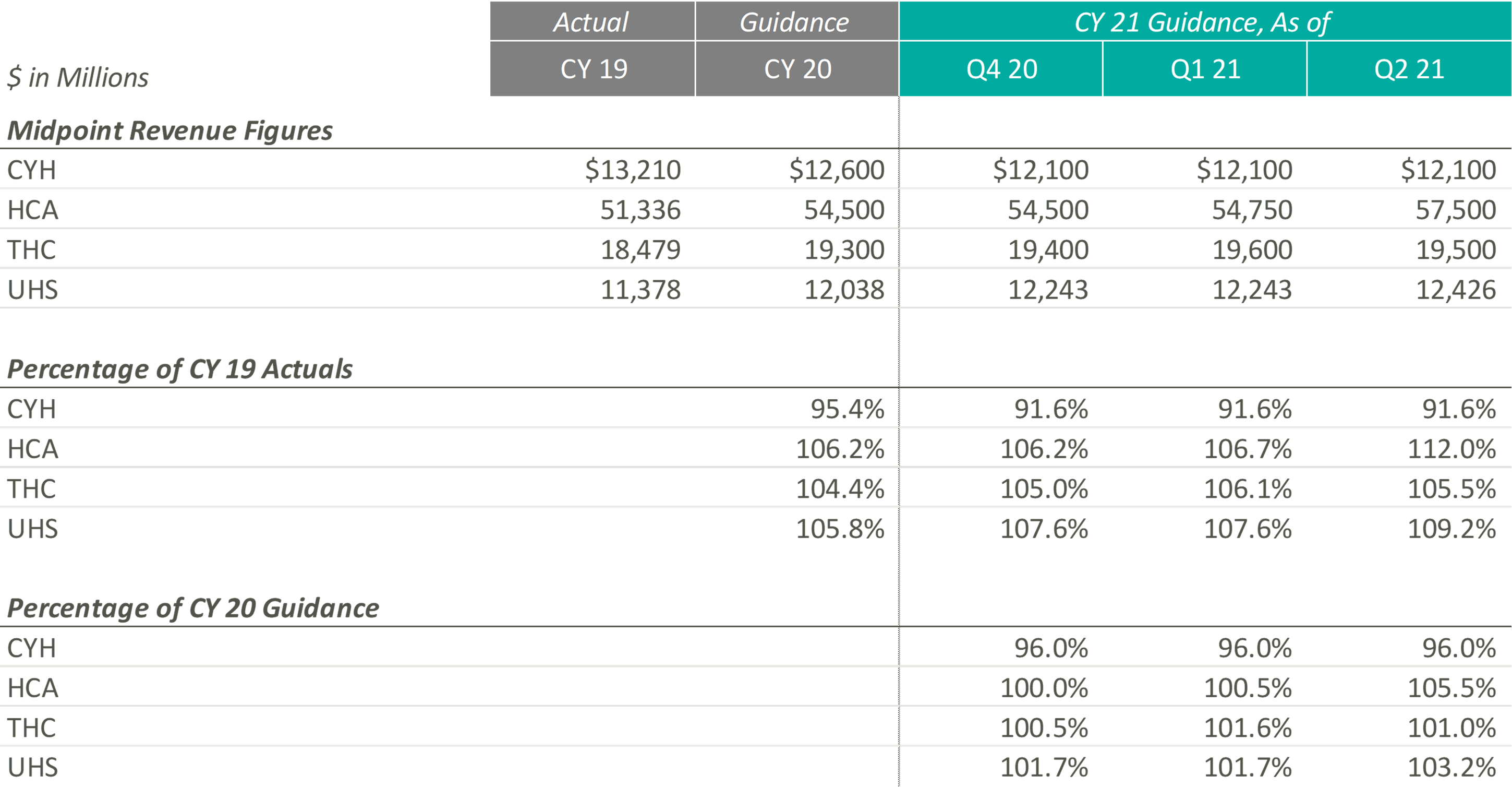
The pandemic’s grip on acute care moderated through Q2 2021 resulting in significant revenue increases for the public hospital operators. Management, often with a tone of surprise, cited strong demand for services as the primary driver of the revenue upticks and reports of double-digit volume growth frequented earnings call highlights.
Samuel N. Hazen, CEO of HCA noted, “On a year-over-year basis, revenues grew 30.0% to $14.4 billion… To highlight a few areas, outpatient surgeries were up 53.0%, emergency room visits grew 40.0%, cardiology procedures increased 41.0%, and urgent care visits were up 82.0%.”
Similarly, Tim L. Hingtgen, CEO and Director of CYH revealed, “For the second quarter, on a same-store basis, net revenue increased 30.2% year-over-year… For the full quarter, year-over-year, same-store admissions increased 17.0%, while adjusted admissions were up 28.5%. Surgeries increased 43.7% and ER visits were up 39.2%.”
As a result of the performance of Q2 2021, public hospital operators further increased their guidance for CY 2021. Still, 2021 revenue guidance remains relatively in-line with pre-COVID 2020 estimates indicating revenue stagnated in 2020. The outlier, CYH, completed a planned divestiture program at the end of 2020, making it difficult to compare post-COVID revenue guidance to the pre-COVID figures.

In terms of profitability, HCA and THC were the earliest Acute Care Hospital operators to predict CY 2021 adjusted EBITDA to exceed the figures estimated at the beginning of CY 2020 and CY 2019, which they publicly estimated as early as Q4 2020. In light of the positive results reported during Q2 2021, CYH and UHS joined their peers in predicting favorable improvements in profitability. As of Q2 2021, the public hospital operators were unanimous in their guidance for the full year in terms of exceeding pre-COVID CY 2020 adjusted EBITDA.
Steve G. Filton, CFO and Secretary of UHS noted, “This robust recovery in volumes exceeded the pace of our original forecast and drove the favorable operating results even in the face of continuing labor pressures in both of our business segments.”
On a margin basis, all Acute Care Hospital operators have estimated CY 2021 adjusted EBITDA margins to exceed CY 2019 and 2020 levels. The pandemic has forced Acute Care Hospitals to take a closer look at their expense structures and streamline operations, leading to the predicted EBITDA margin growth.
The management teams have all reacted positively to a successful first half of 2021, as all four operators expect CY 2021 revenue and adjusted EBITDA levels near or above their initial CY 2021 estimates. However, although the guidance figures seem positive, CY 2021 levels are only at or slightly above pre-COVID CY 2020 expectations, proving that these operators are remaining cautious when providing forward-looking estimates. The Acute Care Hospital industry, while showing signs of recovery after the initial peak of the pandemic, is still experiencing the effects of the COVID crisis, and the recent rise of the Delta variant could further exacerbate the impacts that the COVID-19 pandemic had on the Acute Care Hospital providers.
During UHS’ Q2 2021 earnings call, Steve G. Filton, CFO and Secretary of UHS, cautioned, “During the past 4 to 6 weeks, many of our hospitals have experienced significant surges in the number of COVID patients, and it is not evident that this surge has yet reached its peak. Given the uncertain impact of this most recent surge on non-COVID volumes and on labor shortages, we based our guidance for the second half of the year, primarily on our original internal forecast.”
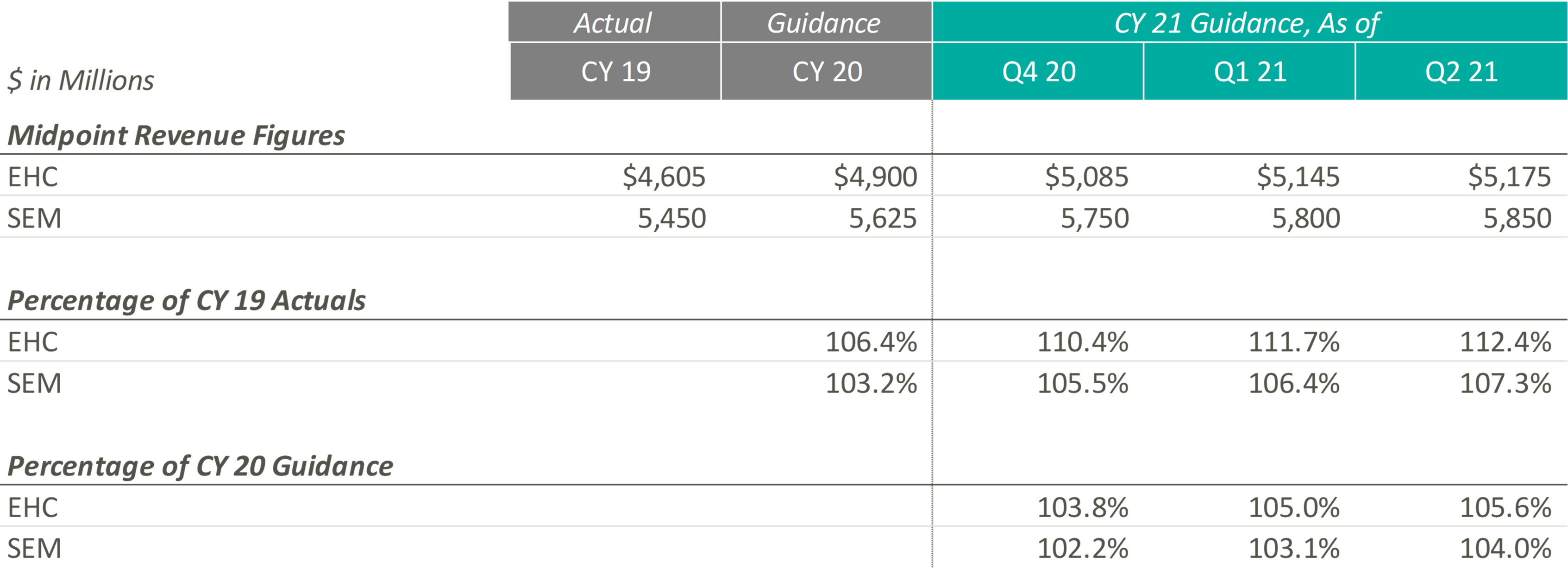
In CY 2021, Post-Acute Care operators expect growth above both CY 2019 revenues and expected pre-COVID CY 2020 revenues. Most notably, when these operators released their original CY 2020 guidance, they projected mid-single digit growth. Looking at their CY 2021 guidance as a percentage of CY 2019 levels and as a percentage of CY 2020, it appears that they expect to still achieve mid-single digit growth on a compounded annual basis from CY 2019. These data points suggest that the Post-Acute Care operators’ growth trajectory was likely not hindered or set back a year by the COVID-19 pandemic.
Additionally, both Post-Acute Care operators have continued to raise their CY 2021 guidance over the past two quarters. During EHC’s most recent earnings call, management highlighted that the return of elective procedures has been fueling inpatient rehabilitation facility (“IRF”) discharge growth. In addition, EHC is experiencing growth in IRF revenue per discharge due to strong reimbursement rates, continued suspension of sequestration, improved discharge destination, and cost report adjustments. These tailwinds, along with the improvement of home health and hospice volumes and IRF M&A activities, resulted in the continued increase of revenue guidance for EHC.
Similarly, SEM has experienced a rebound in volumes in all four segments (i.e., IRFs, long-term acute care hospitals (“LTACHs”), occupational health, and outpatient rehabilitation) at levels well above pre-pandemic levels, resulting in the continued increase in CY 2021 guidance figures. As stated in SEM’s Q1 2021 earnings press release, “In March 2021, both Select Medical’s outpatient rehabilitation clinics and Concentra centers experienced patient visit volume approximating the levels experienced in January and February 2020, the months preceding the widespread emergence of COVID-19 in the United States.”
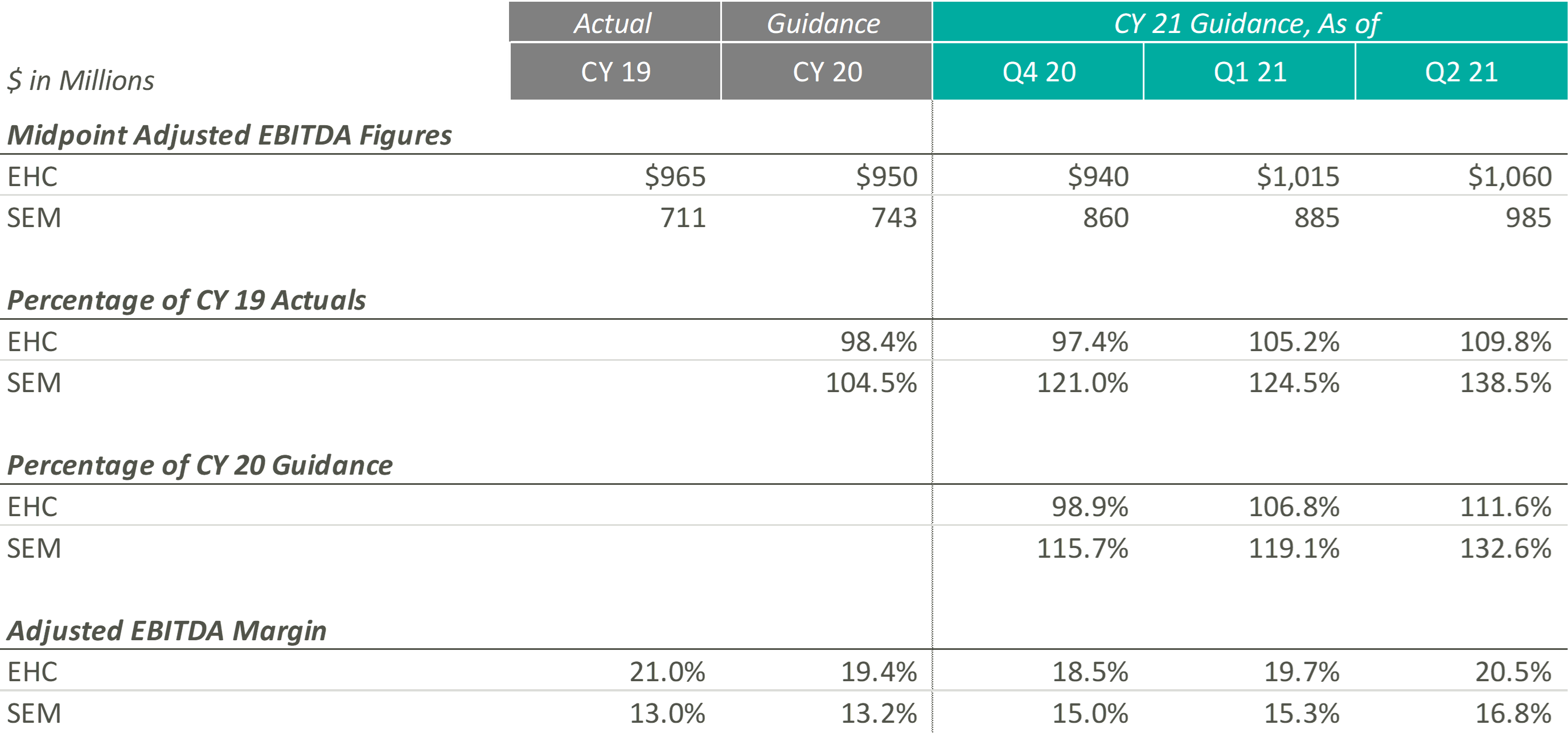
Similar to their CY 2021 revenue guidance figures, EHC and SEM have continued to raise their CY 2021 Adjusted EBITDA guidance ranges. According to EHC’s Q1 2021 earnings release, EHC increased CY 2021 guidance “to reflect Q1 performance and the extension of suspension of sequestration.” Similarly, in Q1 2021, SEM cited revenue growth as the primary driver of adjusted EBITDA growth, with revenue growth resulting from favorable pricing, a new joint venture, a higher acuity patient mix, increased reimbursement rates, and the suspension of sequestration.
Even with the COVID-19 pandemic affecting performance in CY 2020, SEM beat its original CY 2020 midpoint guidance figures by approximately $57.0 million, primarily driven by revenue growth in its inpatient segments. As SEM’s outpatient segments return, SEM’s Adjusted EBITDA performance continues to improve in CY 2021. During SEM’s Q2 2021 earnings call, the Co-Founder & Executive Chairman, Robert A. Ortenzio, stated, “In addition to the volume growth, the inpatient and outpatient rehabilitation hospitals and clinics posted their highest quarters for adjusted EBITDA in the history of the company.”
On the margin side, although EHC has continued to increase its expected CY 2021 Adjusted EBITDA margin throughout the past two quarters, management has cited pressures in nursing staffing across the country that may result in “a little bit of cost climb as we move into 2021 and throughout the year.” On the other hand, SEM has projected Adjusted EBITDA margins at levels well above those expected pre-pandemic. As SEM continues to raise their expected Adjusted EBITDA margin, management has noted that their expenses are being managed well, resulting in current Adjusted EBITDA margins that are “the highest in the history of the company.”
Overall, both Post-Acute Care operators have reacted positively to successful performances over the first half of CY 2021. To this point, Mark Tarr, CEO and President of EHC, noted “the combination of the return of our former market, along with new referral sources we’ve added throughout COVID, leave us very encouraged about the strong organic growth opportunities beginning in the back half of the year.”
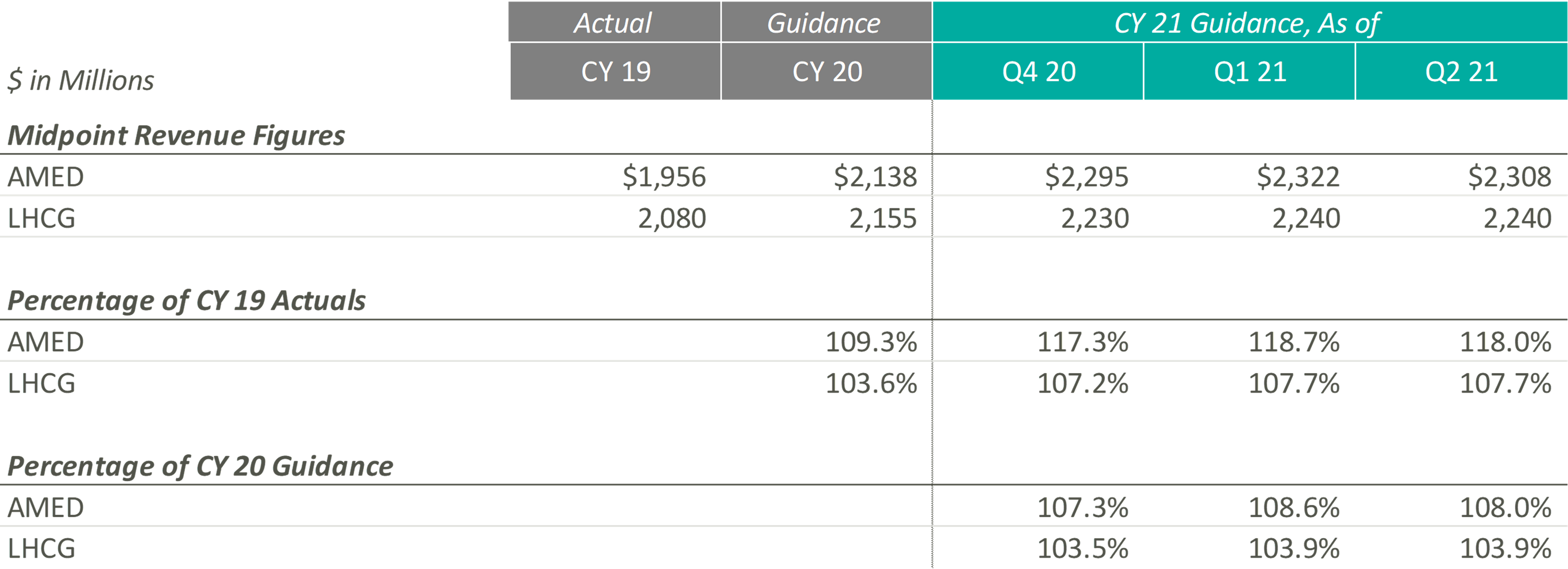
Since the end of CY 2019, AMED and LHCG have both steadily increased their observed revenue estimates, until the most recent quarter. In fact, AMED lowered its CY 2021 guidance during its most recent earnings call citing more conservatism due to the “prolonged, and now, resurgent impact of COVID on our hospice business.” More specifically, the pandemic has resulted in a continued decline and suppression of occupancy rates in senior living facilities (a major referral source), a decrease in length of stay, and an increase in hospice staff turnover. AMED’s management noted that when previously releasing CY 2021 guidance, they had not expected the continuation of COVID impacts during the second half of the year. LHCG discussed similar headwinds but did not adjust the projected guidance figures.
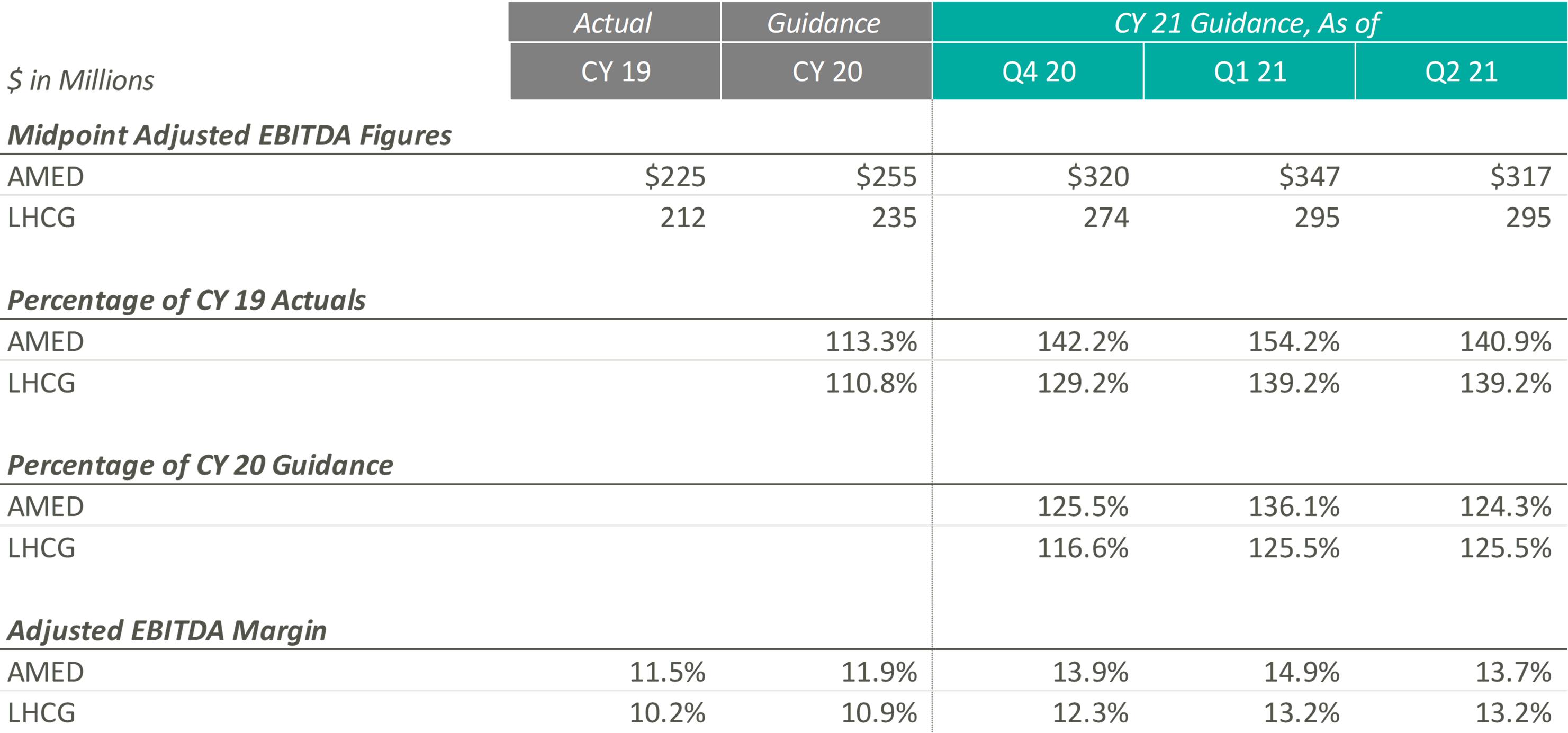
During Q4 2020 and Q1 2021, the Home Health & Hospice operators expected to significantly improve upon their CY 2019 and pre-COVID CY 2020 adjusted EBITDA guidance levels. Keith Myers, CEO of LHCG, discussed the company and overall industry’s success, stating “We are also benefiting from an improved legislative and regulatory outlook as legislative initiatives from Congress, innovation from CMS and stated budget and stimulus priorities of the Biden Administration are all emphasizing the need for at home care.” In addition to improved expected adjusted EBITDA levels since the pandemic, the adjusted EBITDA margin for the Home Health & Hospice operators has also increased compared to CY 2019 and pre-COVID expected CY 2020 levels.
While these Home Health & Hospice operators expected strong performance as they emerge from the pandemic, referrals from senior housing have remained low since the pandemic. Kevin McNamara, CEO and President of Chemed, a company in the space that does not provide guidance for its Home Health & Hospice subsidiary, stated, “The most complex issue still facing [our subsidiary] is the disruptive impact that the pandemic has had on traditional hospice referral sources and low occupancy in senior housing. This disruption continues to impact our admissions and traditional patient census patterns.” This sentiment was reflected in AMED’s Q2 2020 earnings call, where they decreased guidance to reflect the headwinds discussed previously.
Despite the recent concerns related to the continuation of COVID, operators remain optimistic about the future of the space, specifically the demographic tailwinds. During the Q4 2020 earnings call, Paul Kusserow, CEO and President of AMED stated “[Demographics are] in our favor with the baby boomers creating a potential surge of patients in the coming year, with more people turning 65 years old than ever before. The burgeoning 75-plus population, coupled with ever-increasing unsustainable health care costs puts us in a very advantageous position.”
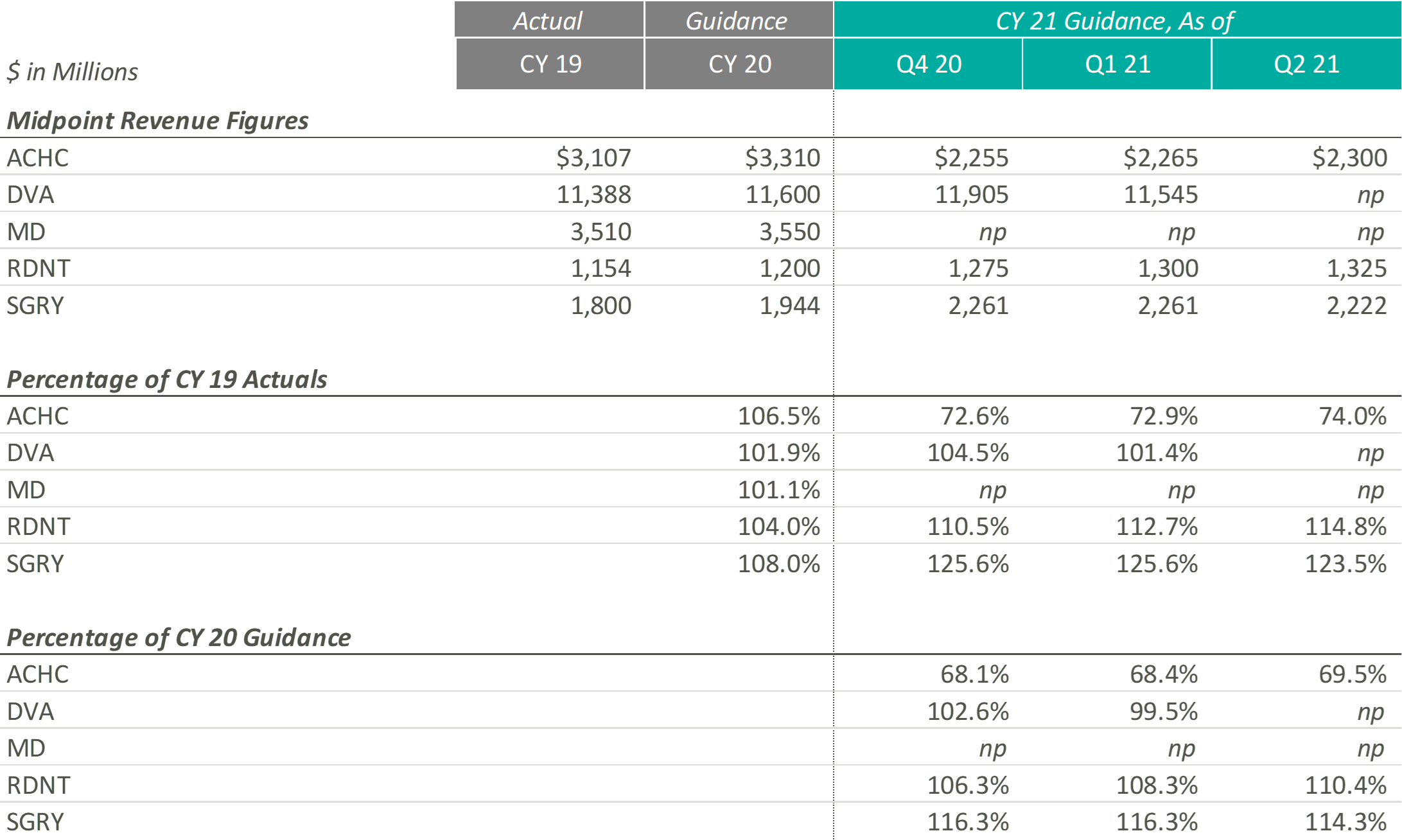
Revenue projections for Outpatient and Other operators are varied as they represent a variety of industries and markets that have been affected by COVID-19 in different ways. RDNT, which provides diagnostic imaging services, and SGRY, which runs ambulatory surgery centers, expect growth above both CY 2019 revenues and expected pre-COVID CY 2020 revenues. RDNT increased their revenue guidance as volume, in virtually all areas of the business, has increased as the states in which they operate have loosened COVID-19 restrictions. While still higher than CY 2019 and CY 2020, SGRY has decreased their CY 2021 revenue guidance as low acuity cases are expected to represent a larger portion of the case mix than previously thought.
On the other end, ACHC, a behavioral health company, expects growth below both CY 2019 revenue and expected pre-COVID CY 2020 revenues. However, ACHC is an outlier as they sold UK operations to a private equity firm in December 2020, making it difficult to compare going forward guidance estimates with historical estimates. ACHC increased CY 2021 guidance as patient volume increased due to the mental health crisis that evolved during the pandemic as well as an increase due to the societal acceptance of mental health services.
DVA, which performs dialysis services, did not provide CY 2021 guidance during the most recent earnings call. Additionally, MD, a physician-led medical group that partners with hospitals, health systems and health care facilities to offer women’s and children’s care, has still not resumed guidance since they announced in their Q1 2020 earnings report that they would no longer provide guidance due to the rapidly evolving nature of the COVID-19 pandemic.
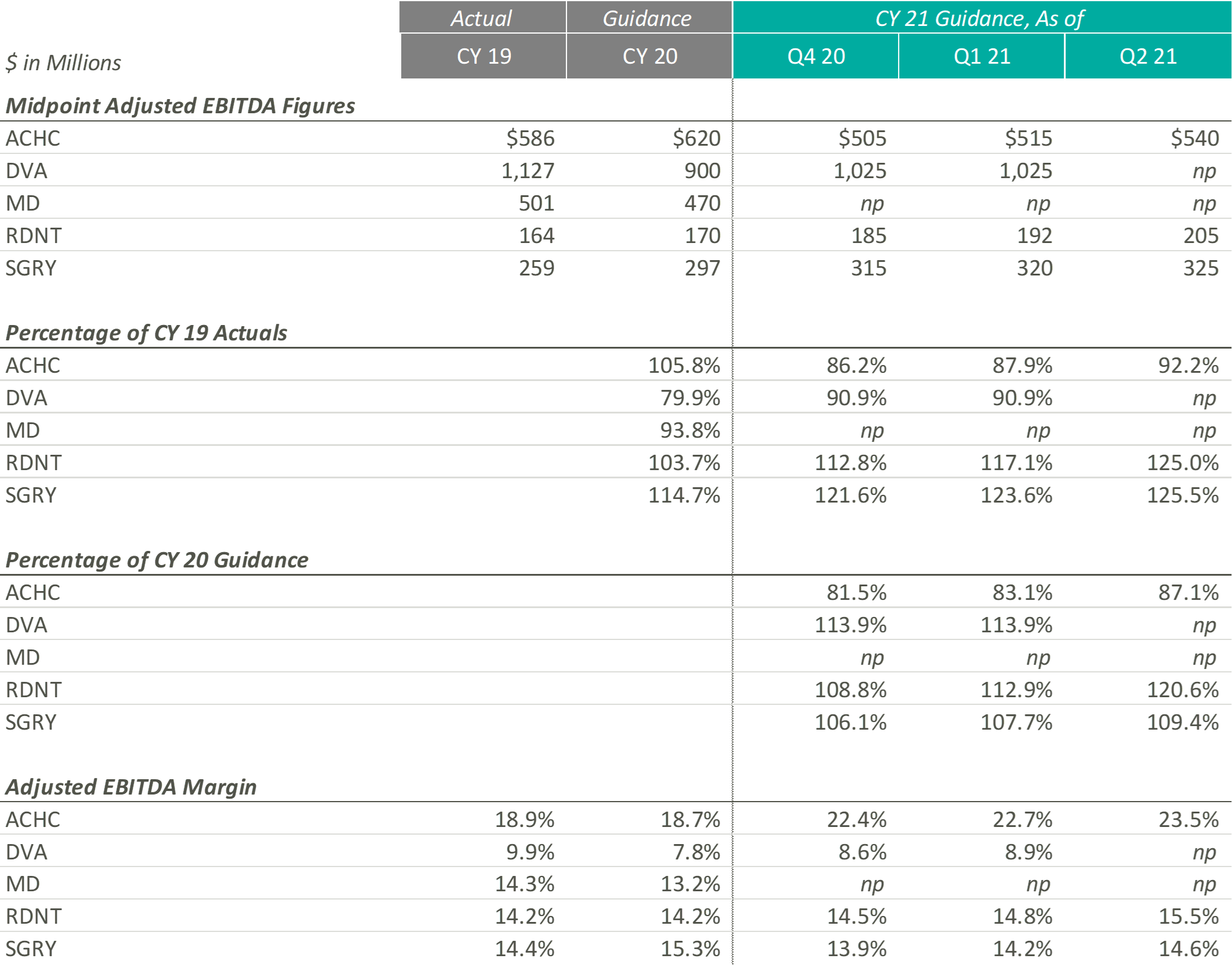
During the most recent earnings calls, every entity that provided guidance increased their CY 2021 guidance figures. ACHC increased adjusted EBITDA guidance due to a rise in patient volume and the expectation that the demand for mental health services is expected to increase. ACHC also expects their adjusted EBITDA margin to increase as more cost synergies are realized with the addition of new beds and facilities.
While DVA did not provide adjusted EBITDA guidance, the CFO & Treasurer, Joel Ackerman, stated “we’re also expecting an uptick on costs related to testing, vaccinations and teammate support as a result of the Delta variants” during the company’s Q2 2021 earnings call.
During the most recent earnings call, RDNT raised their CY 2021 EBITDA guidance from $192m to $205m. According to Mark D. Stolper, the Executive VP & CFO, RDNT’s adjusted EBITDA margins have improved due to regional cost efficiencies and an increase in reimbursement due to previous investments in new equipment. Howard G. Berger, President & CEO of RDNT, recently stated in the company’s Q2 2021 earnings call that “with patient volume returning to more normal levels and through implementing aggressive cost-cutting and cost containment programs, our same-store growth and performance model has returned.”
Like RDNT, SGRY has increased their most recent CY 2021 adjusted EBITDA guidance due to the expectation of volume increases due to seasonality and a rise in higher-acuity procedures. J. Eric Evans, CEO & Director of SGRY, stated in the Q2 2021 earnings call that margins “are projected to increase in the back half of 2021, consistent with historical performance as seasonal commercial mix intensifies.”
The entities in this section represent a variety of sub-industries that were all affected by the pandemic in a unique way. Overall, it appears that the companies that were able to create cost efficiencies and see a notable recovery in volume increase their guidance figures, while those who dealt with increasing expenses and continued volume variability decreased or did not provide guidance.
Although each industry and operator reacted to the pandemic uniquely, the overall outlook among these operators remains positive. Comparing the most recent guidance figures to CY 2019 performance, eight out of eleven operators with sufficient guidance data expect higher revenue in CY 2021 according to their most recent Q2 2021 earnings reports. Furthermore, nine of the same eleven operators estimate similar performance with adjusted EBITDA.
Comparing Q2 2021 guidance to the CY 2020 estimates released before the pandemic can provide additional insight on which companies not only survived but continued to grow throughout the COVID-19 pandemic. Eight out of the eleven operators expect CY 2021 revenue to exceed estimated revenue levels at the beginning of CY 2020. Additionally, ten out of eleven predict similar trends with adjusted EBITDA. However, it is interesting to note that some of these operators, specifically in the Acute Care Hospital sectors, expect CY 2021 estimates to outperform CY 2020 estimates only by a slim margin. Since these operators are only predicting a small amount of revenue and adjusted EBITDA margin expansion from 2020 to 2021, it appears they might not have experienced normal levels of development throughout the pandemic. The Post-Acute Care and Home Health & Hospice operators, on the contrary, expect to significantly outperform pre-COVID CY 2020 estimates in 2021, illustrating that these two sub-industries may not have experienced a “lost year” of growth in 2020 as a result of the COVID-19 pandemic.
Lastly, to understand how these operators’ performance has trended throughout CY 2021, we have compared the most recent CY 2021 guidance figures to those released during the Q4 2020 earnings calls. Nine out of eleven companies have adjusted revenue guidance to levels at or above the initial figures, and ten out of the eleven have either increased adjusted EBITDA estimates or left them equal. Based on these statistics, it appears operators have successfully started CY 2021.
Despite the lingering COVID-19 pandemic, it appears healthcare operators are optimistic about the recovery of their revenue and Adjusted EBITDA metrics over pre-pandemic levels. Further, many healthcare operators have taken the past year and a half to implement new strategies that will allow them to become more efficient long-term. Overall, it appears the healthcare operators have adapted during these times and are optimistic about their future performance despite the lingering COVID-19 pandemic.
Authors
Related Content