- About Us
- Our Clients
- Services
- Insights
- Healthcare Sectors
- Ambulatory Surgery Centers
- Behavioral Health
- Dialysis
- Hospital-Based Medicine
- Hospitals
- Imaging & Radiology
- Laboratories
- Medical Device & Life Sciences
- Medical Transport
- Oncology
- Pharmacy
- Physician Practices
- Post-Acute Care
- Risk-Bearing Organizations & Health Plans
- Telehealth & Healthcare IT
- Urgent Care & Free Standing EDs
- Careers
- Contact Us
The Risks and Rewards of Setting Physician Compensation Internally
Published by Healthcare Financial Management Association
A rapid growth in physician alignment strategies has created a surge in physician service agreements.
To maintain compliance with regulatory guidance from the Centers for Medicare & Medicaid Services (CMS), the Office of Inspector General (OIG), and other authorities, hospital leaders should set physician compensation at fair market value (FMV). FMV is defined in the professional literature as “the price, expressed in terms of cash equivalents, at which a property would change hands between a hypothetical willing and able buyer and a hypothetical willing and able seller, acting at arm’s-length in an open and unrestricted market, when neither is under compulsion to buy nor to sell, and when both have reasonable knowledge of the relevant facts.”a
Although some hospitals might consider hiring a third-party firm to determine whether each physician arrangement is at FMV, this approach can be time-consuming and expensive. Fortunately, healthcare executives also have a choice of various other strategies that can streamline this process and, if implemented properly, solidify compliance efforts within the health system.
Compliance Essentials
Health systems should consider taking clear steps to demonstrate a commitment to compliance. The mere existence of a compliance program that outlines how to set physician compensation, for example, can demonstrate the health system’s good-faith intent to comply with the FMV standard. This program should promulgate written protocols and best practices, and it should be effectively communicated throughout the organization, with staff assigned to monitor and, most important, enforce the program. When physician compensation is set through an inconsistent process throughout a health system, such as via business development initiatives, the arrangement is more likely to be subject to regulatory scrutiny. Click to continue to the full article.Five Guidelines for a Compliant Shared Savings Arrangement
Published by Compliance Today
Through the development of Accountable Care Organizations (ACOs) and other third-party payer programs, cost savings arrangements between hospitals and physicians are becoming an increasingly important tool for the efficient operation of hospital service lines and outpatient clinics. Historically, similarly structured agreements, such as gainsharing arrangements, have been scrutinized by the Office of the Inspector General (OIG) for a multitude of reasons. However, there have been numerous favorable OIG Advisory Opinions related to these arrangements. From these opinions, one can identify guidelines for a compliant shared savings agreement. This article will address five pertinent guidelines related to shared savings arrangements that a hospital should consider.
1. Patient safety parameters
Certain safeguards should be in place to protect the patient population. Legal counsel typically includes these parameters to ensure the quality of care will not be negatively affected by the program. A few key points from the favorable OIG opinions related to this initiative are:- The arrangement should be administered by a program administrator whose compensation is not related in any way to the cost savings agreement or physicians’ compensation.
- The program should contain significant safeguards to protect against inappropriate reductions or limitations in services.
- The program should have an independent reviewer or auditor review the program prior to commencement and at least once per year.
- Patients treated under the arrangement should have their care monitored by a quality or safety committee.
- Written disclosure of the program should be provided to patients prior to admission or prior to the approval of the relevant procedure.
Correlating Industry Trends With Imaging-Center Value
Published by ImagingBiz
While consideration of the individual facts, circumstances, and local competitive position of each subject imaging center is integral to an accurate business-valuation analysis, a thorough understanding of the state of the imaging industry—particularly the acquisition environment—is crucial to performing an accurate and complete valuation. Radiology Business Journal recently published the results of its third annual survey¹ related to the top 20 imaging-center chains and the larger economic environment in which they operate. These data can be used to gain a better understanding of how the valuation of imaging centers will trend in 2013 (and beyond). Industry data, such as those in the imaging-center–chain survey, are very important to valuation analysis. Properly incorporating such industry data into the key assumptions and components of the valuation transforms the valuation analysis from a mathematical exercise into a meaningful and useful assessment of the market value of the subject imaging center.
As the trend toward consolidation in the marketplace continues, it will be critical for owners of imaging centers to understand the value of their organizations fully—the better to assess their options as the marketplace evolves.
Key Valuation Takeaways
Many trends identified in the survey are positive, from a valuation perspective. As in the past nine out of 10 years, the number of total imaging centers increased in 2012. This increase in total imaging capacity is interesting, given the challenging reimbursement environment, and might be attributable to an anticipated increase in total patient volume following the implementation of the individual mandate of the Patient Protection and Affordable Care Act in 2014. The imaging-center chains that made it into the top 20 remained stable, signifying that large industry players are maintaining and/or growing their strength in the marketplace. In total, the top 20 companies increased the number of centers owned by over 100 centers. It is interesting that a large number of the additions were acquisitions, indicating that there is clearly an active market for imaging centers. This active market is a hallmark of a healthy industry. The data in surveys such as this can provide assistance to the valuation analyst in formulating a basis for both growth assumptions and acquisition-market conditions. Click to continue to the full article.4 Factors Affecting ASC Valuation and Sales
Published by Becker's ASC Review
With contributions from Colin McDermott, CFA, CPA/ABV
Surgery center owners looking to sell should be aware of several factors influencing valuation and profitability.
Colin McDermott, CFA, CPA, is a senior manager with VMG Health in Dallas. He specializes in providing financial, valuation and transaction advisory services to healthcare clients, including ambulatory surgery centers and hospital systems.
Here are Mr. McDermott's four main factors affecting ASC valuation and sales.
Click to continue to the full article.
Hospital Operators ACO Quotes: Lay the Groundwork, or Wait and See?
Published by Becker's Hospital Review
Since the Affordable Care Act of 2010 sanctioned the development of accountable care organizations (“ACOs”), healthcare groups have been divided on whether or not to participate.
While some industry leaders view the initiative as an opportunity to lower the cost of healthcare, others view ACOs as nothing more than a modernized version of capitation. The following public statements made by public company hospital executives highlight the sentiment of healthcare systems that are laying the groundwork for ACOs and those that are waiting until reliable evidence of actual cost savings is available.
Click to continue to the full article.
Commercially Reasonable – Whose Responsibility is it?
Published by Healthcare Financial Management Association
Hospital finance executives can play an important role in assessing whether proposed transactions between their organizations and physicians meet regulatory standards for being commercially reasonable.
The healthcare industry has experienced significant growth in the number and types of physician integration strategies. Obvious reasons, such as declining payment, expensive IT, and anticipation of new payment methods based on quality and cost savings, are prompting both physicians and hospitals to consider new arrangements to work together. Some of these strategies have existed for years (e.g., medical directorships and direct employment), while others are relatively new (e.g., compensating physicians for quality). Regardless of the arrangement type, when hospital or health system executives contemplate entering into an agreement with a physician or physicians, they must be mindful of federal regulations mandating that these arrangements be commercially reasonable. Failure to do so could result in civil monetary penalties (see sidebar on page 2).
Determining whether an arrangement between a hospital and a physician is commercially reasonable can be challenging. It requires an understanding of a healthcare facility’s operational needs, clinical requirements, and
financial alternatives. Expertise in healthcare valuation and healthcare law is also needed because compensation under an arrangement deemed to be commercially reasonable must be set at fair market value (FMV) and the agreement must be structured to be consistent with regulatory guidance.
In short, healthcare executives should understand the key considerations that attorneys and valuation firms explore as they assess whether an arrangement is commercially reasonable. Following are some of these considerations.
Click to continue to the full article.
Intellimarker™ Trends: Staffing Expenses and Efficiencies
The following article was written by Chance Sherer, manager with VMG Health.
For the past five years, VMG Health has published the Multi-Specialty ASC Intellimarker™ Financial & Operational Benchmarking Study (the "Intellimarker™"), which provides detailed financial benchmarking information and analyses on ASCs around the United States. The Intellimarker™ is designed to help industry insiders better understand the relative financial and operating performance of ASCs. The Intellimarker™'s data also may help pinpoint issues and provide a basis for developing operational strategies to improve financial performance and creating value. By reviewing the Intellimarker™ data over time, we have been able to identify certain trends in the ASC industry.
Today, ASCs are facing increasing reimbursement pressure and compete with one another for patients and physicians. ASC owners and operators are focusing on expense management as a way to increase profitability and distributions, thereby making the ASC more attractive to current and potential physician investors.
Click to continue to the full article.
The Income Approach: Valuing Real Estate vs Valuing a Business
Published by Becker's Hospital Review
Valuations of a business or enterprise and real estate share numerous methodologies, terms and standards, which often result in confusion amongst the distinct disciplines. Both types of valuation largely depend upon an Income Approach. Both utilize financials that are usually prepared and audited by a third-party and in accord with Generally Accepted Accounting Principles (“GAAP”). Both valuations depend upon an appraiser’s ability to determine either a stabilized income stream or to prepare a reasonable forecast based upon historical performances, current market conditions and projected future market conditions.
Business valuations utilize EBITDA (earnings before interest, taxes, depreciation and amortization) as a key format metric to determine value. An appraiser’s ability to either determine a stabilized level of EBITDA or a reasonable forecast of EBITDA then allows for the application of a market-derived multiple or a discounted cash flow analysis in order to determine a supportable determination of value.
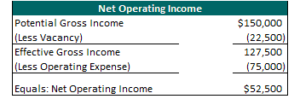
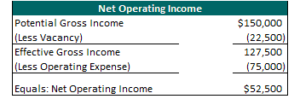
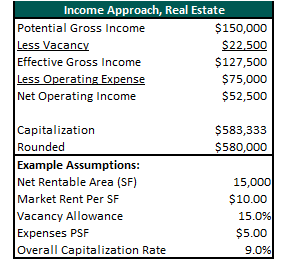
Within the context of a real estate analysis, Net Operating Income is the key formula metric of value that parallels EBITDA for business valuation. Please note that the Net Operating Income is exclusive to the operation of the real estate component only. An example of a Net Operating Income calculation is depicted in the following table.
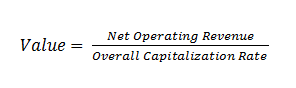
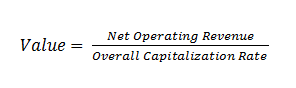
 Once the appraiser's estimate of net operating income is made, two options to convert this into an indication of value are available. If the net operating income is considered to be at a stabilized value, then the application of an overall capitalization rate is often utilized. An overall capitalization rate is an arithmetic factor that expresses the relationship between net operating income and value through division. The calculation is expressed as:
Once the appraiser's estimate of net operating income is made, two options to convert this into an indication of value are available. If the net operating income is considered to be at a stabilized value, then the application of an overall capitalization rate is often utilized. An overall capitalization rate is an arithmetic factor that expresses the relationship between net operating income and value through division. The calculation is expressed as:
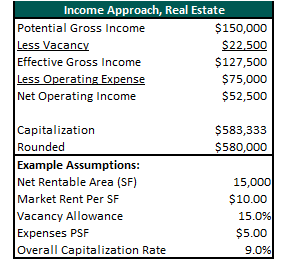
 There are several methods of extracting an Overall Capitalization Rate. The most prominent cap rates are abstractions directly from the marketplace itself. By dividing a comparable property’s net operating income by the sale price, an Overall Capitalization Rate can be derived. These rates then can be compared to the subject property in terms of the quantity, quality, and durability of the income streams. Other popular methods of Overall Capitalization Rate derivation include market surveys (from appraiser or published surveys), the band-of-investment technique, and debt coverage rate analysis. The following table depicts an example of the methodology employed in the Income Approach of real estate.
If a Net Operating Income stream is not stabilized, then a discounted cash flow analysis is often preferred in the analysis of real estate.
There are several methods of extracting an Overall Capitalization Rate. The most prominent cap rates are abstractions directly from the marketplace itself. By dividing a comparable property’s net operating income by the sale price, an Overall Capitalization Rate can be derived. These rates then can be compared to the subject property in terms of the quantity, quality, and durability of the income streams. Other popular methods of Overall Capitalization Rate derivation include market surveys (from appraiser or published surveys), the band-of-investment technique, and debt coverage rate analysis. The following table depicts an example of the methodology employed in the Income Approach of real estate.
If a Net Operating Income stream is not stabilized, then a discounted cash flow analysis is often preferred in the analysis of real estate.
 In summary, both business valuations and real estate valuations often rely upon an Income Approach to generate value. Both sciences base value upon the determination of either stabilized income stream or a reasonable forecast of income. However, each of the disciplines utilize a separate and distinct methodology and base financial metric in the final derivation of value.
Click to continue to the full article.
In summary, both business valuations and real estate valuations often rely upon an Income Approach to generate value. Both sciences base value upon the determination of either stabilized income stream or a reasonable forecast of income. However, each of the disciplines utilize a separate and distinct methodology and base financial metric in the final derivation of value.
Click to continue to the full article.
 Once the appraiser's estimate of net operating income is made, two options to convert this into an indication of value are available. If the net operating income is considered to be at a stabilized value, then the application of an overall capitalization rate is often utilized. An overall capitalization rate is an arithmetic factor that expresses the relationship between net operating income and value through division. The calculation is expressed as:
Once the appraiser's estimate of net operating income is made, two options to convert this into an indication of value are available. If the net operating income is considered to be at a stabilized value, then the application of an overall capitalization rate is often utilized. An overall capitalization rate is an arithmetic factor that expresses the relationship between net operating income and value through division. The calculation is expressed as:
 There are several methods of extracting an Overall Capitalization Rate. The most prominent cap rates are abstractions directly from the marketplace itself. By dividing a comparable property’s net operating income by the sale price, an Overall Capitalization Rate can be derived. These rates then can be compared to the subject property in terms of the quantity, quality, and durability of the income streams. Other popular methods of Overall Capitalization Rate derivation include market surveys (from appraiser or published surveys), the band-of-investment technique, and debt coverage rate analysis. The following table depicts an example of the methodology employed in the Income Approach of real estate.
If a Net Operating Income stream is not stabilized, then a discounted cash flow analysis is often preferred in the analysis of real estate.
There are several methods of extracting an Overall Capitalization Rate. The most prominent cap rates are abstractions directly from the marketplace itself. By dividing a comparable property’s net operating income by the sale price, an Overall Capitalization Rate can be derived. These rates then can be compared to the subject property in terms of the quantity, quality, and durability of the income streams. Other popular methods of Overall Capitalization Rate derivation include market surveys (from appraiser or published surveys), the band-of-investment technique, and debt coverage rate analysis. The following table depicts an example of the methodology employed in the Income Approach of real estate.
If a Net Operating Income stream is not stabilized, then a discounted cash flow analysis is often preferred in the analysis of real estate.
 In summary, both business valuations and real estate valuations often rely upon an Income Approach to generate value. Both sciences base value upon the determination of either stabilized income stream or a reasonable forecast of income. However, each of the disciplines utilize a separate and distinct methodology and base financial metric in the final derivation of value.
Click to continue to the full article.
In summary, both business valuations and real estate valuations often rely upon an Income Approach to generate value. Both sciences base value upon the determination of either stabilized income stream or a reasonable forecast of income. However, each of the disciplines utilize a separate and distinct methodology and base financial metric in the final derivation of value.
Click to continue to the full article.3 Methods for Managing Concern in a Community Hospital Acquisition
Published by Becker's Hospital Review
A community-owned hospital is often the largest asset of the community. Unfortunately, with decreasing reimbursement and climbing costs, more and more community hospitals have been struggling. Residents need a local hospital to remain operationally viable in order to protect local access to healthcare services. For this reason, an increasing amount of community hospitals have been looking to hospital operators or large health systems to partner and/or acquire them, evidenced by the influx in hospital mergers and acquisitions over the past few years.
Concern is high with hospital acquisitions, buyouts of community hospitals When a local hospital is acquired it can raise concerns among the residents, hospital employees and physicians. "Residents can be very leery of somebody coming in from the outside and buying their largest asset — the local hospital. Apprehension is high with staff, community residents and physicians," says Jim Rolfe, managing director of VMG Health's transactional services division.
Click to continue to the full article.
Financial Drivers of ASC Success
Published by SurgiStrategies
Proactively managed ASCs continue to look for ways to remain competitive, financially, operationally and strategically. The ASC industry is not only facing a maturation of its industry, but is also dealing with a sluggish economy which continues to impact volumes. Therefore volume and revenue growth are challenging in this environment. In addition, physicians are retiring at a faster rate than new physicians are entering the market. This trend is expected to continue as baby boomers reach retirement age. Furthermore, uncertainty surrounding healthcare reform’s long-term impact on ASCs still exists. There is no question that managed care and Medicare will continue to present reimbursement pressure and therefore net revenue per case (NRPC) will likely continue to decline. Given the maturation of the industry, a sluggish economy, physician shortage and pressure from payors, successful ASCs will be forced to identify ways to capture the right volume, stay ahead of the cost curve and proactively address legislative headwinds. There are a few strategies an ASC should be actively considering in order to drive financial success: increase revenue as it relates to price and volume, and decrease fixed and variable expenses.
