
Private Equity Investment in Ambulatory Surgery Centers
Rachel Linch
September 21, 2023
Effective January 16, 2024, Compliance Risk Analyzer has joined VMG Health. Learn more.
October 19, 2023
Written by Matthew Marconcini, CPA and Lukas Recio, CPA
In recent years, there has been a notable surge in hospitals and healthcare systems entering into joint ventures with private equity groups. This trend is driven by several different factors that reflect the ever-evolving landscape of the healthcare industry and it is expected to continue in the future.
Howard G. Berger, CEO and Board Chairman of RadNet, said, “Another one of our significant initiatives is expansion through hospital and health system joint ventures. In the past, we have stated that we see a path forward towards holding as much as 50% of our imaging centers in these partnerships.”
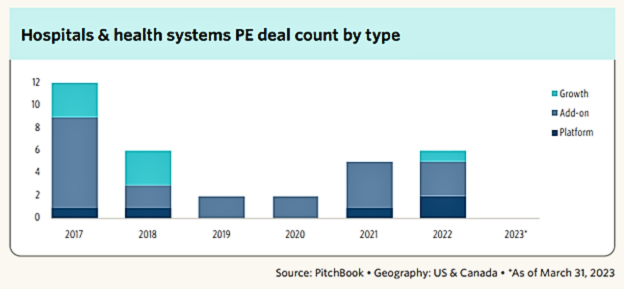
Additionally, based on the graph below, we can see there has been a continued increase from 2019 to 2022 in PE deal count for hospitals and health systems.
Firstly, the financial pressures faced by many healthcare providers have led them to seek external investments to bolster their resources. Private equity groups, with their substantial capital reserves, offer a lifeline to struggling hospitals, and enable them to invest in technology, infrastructure, and quality improvement initiatives.
Secondly, private equity firms bring expertise in business management and operational efficiency to the partnership. In an increasingly competitive healthcare environment, hospitals and health systems must find ways to streamline operations, reduce costs, and enhance patient care. Partnering with private equity allows healthcare organizations to tap into the financial and operational acumen of their partners which leads to more effective and efficient healthcare delivery. For instance, we have seen hospitals create joint ventures within their behavioral health operations because they want to keep the service but need to bring in a partner that has the financial resources and operational expertise to help turn it around. Another area where we have seen an increase in successful partnerships with private equity is hospitals looking for a better urgent care strategy. Private equity has the resources, financial backing, and expertise to bring in the right systems and people to create substantial value. Private equity firms help urgent care clinics standardize processes, consolidate overhead costs, and find new branch locations without saturating the market. This assistance helps relieve physicians from tasks that they are typically too busy to tackle.
Moreover, the shift towards value-based care models has necessitated investments in population health management and preventive care. Private equity investments can provide the necessary funds to develop and implement the necessary tools to accurately estimate the total cost of care with the goal of delivering better patient outcomes and increased cost savings in the long run.
Lastly, the COVID-19 pandemic exposed vulnerabilities in healthcare infrastructure and underscored the need for agile, resilient healthcare systems. Private equity partnerships can help healthcare providers strengthen their resilience, enhance their preparedness for future crises, and adapt to the rapidly changing healthcare landscape.
While there are many benefits hospitals are seeing by partnering with private equity groups, there are several areas, listed below, that need to be discussed between the parties as they consider this partnership:
In conclusion, the increasing collaboration between hospitals and health systems with private equity groups is a response to the multifaceted challenges and opportunities in the healthcare sector. These partnerships offer financial flexibility, operational expertise, and a pathway to innovation. All of these offerings are essential for healthcare organizations striving to provide high-quality care in a rapidly evolving marketplace. As healthcare continues to transform, such joint ventures are likely to remain a key strategy for hospitals looking to thrive in the years ahead.
October 18, 2023
Written by Kyle Spears and Nicole Montanaro, CVA
Per the U.S. Healthcare Staffing Market Size, Share & Trends Analysis Report, the U.S. healthcare staffing market is expected to reach USD 34.7 billion by 2030. The growing demand for healthcare staffing services has driven the rise in service agreements among related parties, some of which require a fair market value opinion. The underlying reasons for this high demand include:
Additionally, according to the U.S. Bureau of Labor Statistics’ Occupational Outlook Handbook, employment is expected to grow from 2022-2032 for registered nurses (6%), nurse anesthetists, nurse midwives, nurse practitioners (38%), physician assistants (27%), physical therapists (15%), occupational therapists (12%), speech-language pathologists (19%), EMTs and paramedics (5%), and physicians and surgeons (3%).
With this growing demand for healthcare workers, healthcare operators are increasingly seeking new ways to staff their facilities. For example, many have outsourced recruitment and staffing operations to third-party healthcare staffing firms. Another popular solution includes entering into third-party agreements and/or partnerships with other health systems, hospitals, and outpatient facilities that have a greater scope of in-house operations and better access to qualified talent.
The latter is often between parties that may be able to refer to one another which adds a layer of complexity to these arrangements. As with many healthcare arrangements, the fair market value requirement becomes an important part of the process before signing one of these agreements. As discussed in more detail below, VMG Health has provided insight as to what leaders should think through when entering into recruiting and leased staff agreements with related parties.
The typical recruiting services arrangement will include either a retained fee (payment made up-front) or a contingent fee (payment made upon placement) that is stated as a percentage of the candidate’s first-year salary.
Although recruiting services for various position levels (i.e., physicians, advanced practice providers, nurses, senior management, etc.) can be provided by the same personnel or service providers, it is important to note that the fees for each position level often vary based on factors including, but not limited to, the size of the qualified candidate pool, difficulty to recruit a certain position in a certain market, and the skill/expertise required of the candidate. Therefore, many recruiting services agreements will include a specific fee for each position level rather than one encompassing fee for all positions.
Due to the various scope of services and positions recruited, it may be difficult to find agreements in the market that could be considered directly comparable to a party’s recruiting needs. Therefore, from a valuation and compliance perspective, it is also important to consider the service provider’s costs to provide the recruiting services in addition to observed market fees, if available. This two-step process helps the contracting parties truly understand what services are being provided and assists with documenting FMV.
Similar to recruiting services, leased staff arrangements are highly tailored to both the specific needs of one party and the staffing availability of the service provider. That said, the fee structure for these arrangements is often based on a markup to the fully loaded personnel costs, in which the appropriate markup to costs varies depending on the nature of the staffing arrangement and the financial risk placed on the service provider.
From a high-level perspective, an important factor for a staffing arrangement is the nature in which the personnel will be provided, as laid out below:
Additionally, factors such as the contract period of the agreement, payment terms (actual costs vs. projected costs), and type of staff provided (clinical personnel or administrative personnel), may impact the financial risk placed on the service provider under the arrangement.
As the demand for competent healthcare staff continues to grow, healthcare leaders are identifying numerous types of companies that can fulfill their staffing needs. Since many of these companies are in a position to refer, it is important to ensure any recruiting and leased staff agreements are consistent with FMV principles. VMG Health has extensive experience valuing FMV payments for recruiting services and leased staff arrangements.
October 12, 2023
The following article was published by Becker’s Hospital Review.
Private equity (PE) investment in healthcare is soaring, as investors have raised large amounts of capital and see attractive opportunities in the industry — especially health services.
At the same time, while hospital and health system leaders grapple with narrow operating margins and limited resources, they see exciting possibilities in partnership and joint ventures with PE-based platforms.
To better understand the forces behind these trends, Becker’s Hospital Review recently spoke with Greg Koonsman, founder and CEO of VMG Health, a full-service healthcare advisory firm with extensive knowledge and expertise related to PE investments in healthcare services.
There is $7.6 trillion in PE globally, according to a recent McKinsey report. According to Mr. Koonsman, these funds have grown significantly over the past 15 years, as many institutional investors have increased their allocation of assets to this asset class. As institutional allocations to private capital have swelled, the number of private capital fund managers has grown from 3,700 to more than 13,000.
In the U.S., where healthcare represents about 20 percent of the economy, a proportional amount of PE is allocated to healthcare investments, representing about $500 billion. Of the PE funds allocated to healthcare, Mr. Koonsman estimates that at any given point, there is between $80 and $120 billion in “dry capital” waiting to be invested.
“The sheer size of the market has driven the increased interest in activity by private equity in healthcare services,” Mr. Koonsman said.
In the late 1990s and early 2000s, many PE firms shied away from healthcare services, Mr. Koonsman said. Their reluctance stemmed from the regulatory environment; the presence of nonprofit health systems, which dominated the market; and the powerful role of physicians. “For many years, healthcare services was, in a sense, avoided by many firms,” Mr. Koonsman said.
But in the past 15 years, more PE firms have started to invest in areas adjacent to the core of healthcare, as seen in veterinary medicine, dermatology, ophthalmology, contract research organizations and other ancillary healthcare services. “The oversupply of capital, together with the fact that private equity firms have gotten more accustomed to understanding the nuances of healthcare services and the regulatory environment, has resulted in more investments in healthcare services,” Mr. Koonsman said.
Now, PE firms are going a step further. They’re increasingly investing in healthcare services that are more fundamental to a health system’s core business. This includes investments in diagnostic imaging, ambulatory surgery, cancer treatment, and physician practices in areas like orthopedics, cardiology, primary care multispecialty care and urgent care.
Even with the economic challenges of recent years, PE investment in healthcare has remained strong. An April 2023 Becker’s Healthcare article highlighted key data from consulting firm Bain & Co: In 2021, $151 billion was invested in PE healthcare deals, followed by $90 billion in 2022 — the second-highest year on record. Mr. Koonsman expects this trend to continue in late 2023 and 2024.
As PE firms increasingly eye investments in areas of healthcare that have traditionally been core to hospitals and health systems — and hospitals and health systems struggle to grow in this capital-constrained environment — more discussions are transpiring between health systems and PE funds (or PE-backed platforms) about mutually beneficial partnerships and joint ventures.
Based on his extensive exposure to these types of partnerships and joint ventures, Mr. Koonsman sees immense benefits for both healthcare organizations and PE investors.
Health systems have strong, trusted brands within local geographies; size, scale and leverage within their respective markets; years of data; and relationships at all points in the provider chain. However, health systems, which typically provide services in dozens of verticals, have difficulty allocating their existing capital across multiple areas, lack sufficient capital for growth opportunities and lack the focus and management expertise to capitalize on promising opportunities.
These shortcomings are areas where PE funds and PE-backed platforms can bring tremendous value. PE has access to significant capital and excels in building professional management teams with a laser focus on specific growth opportunities. This combination of capital, management expertise and focus can accelerate the speed of maximizing growth opportunities and value.
“I think when you put those positive attributes together, a very good partnership can be developed,” Mr. Koonsman said.
However, in building successful partnerships, there will be obstacles. Among them is achieving alignment. Mr. Koonsman has found that PE firms often lack a deep understanding of health systems, especially nonprofit systems, and health systems often don’t understand or appreciate the value of a PE platform. When these parties make efforts to better understand one another’s goals, strengths and time horizons, misconceptions or knowledge gaps can be reconciled.
Further, a health system might consider participating as an investor in a PE platform. This provides the health system with insight to the benefits of the partnership and the equity value created. “It has been a mistake for health systems to create significant value in a platform without participating in this value,” Mr. Koonsman said. “There is an opportunity for a health system to create value in their local market through the partnership itself and also participate in a national platform that’s going to create outsized returns for their investment.”
Generally speaking, the types of PE firms looking at investments in healthcare services are funds with $500 million to $5 billion (middle market private equity) to invest. When considering a potential investor, health systems should look carefully for partners with a significant focus on healthcare. “Having a firm that understands healthcare is critical,” Mr. Koonsman said. “I would say that probably the experience and expertise in healthcare is the most important differentiator.”
It’s also critical that health systems look for “partnership-oriented firms.” Some investors will purchase 90 to 100 percent of a firm and then behave as an autocrat, which is not the type of a partner a health system wants. Health systems want investors who are collaborative and partnership-oriented. This is essential.
Mr. Koonsman said these partnerships are only going to expand. “They are fundamentally a part of the future of health systems,” he said, adding that he foresees more partnerships involving physician organizations in various specialties, including musculoskeletal, cardiology, oncology, OB-GYN, primary care, urgent care, post-acute care and more.
He envisions a new form of three-way partnership emerging that involves the health system, physicians and a PE-based platform. “I think there’s an opportunity for realignment of the relationship between health systems, physicians and private equity,” he said. “I think there’s a way the health system can accomplish their strategic objectives with their physician partners and roll them back into more of an ownership position alongside private equity-based businesses — almost like a three-way venture that realigns everyone’s economic interests.” While complex, such partnerships are possible, with the ambulatory surgery center business providing a prime example, he said.
There is significant opportunity in PE investments in healthcare today, given the tremendous amount of uninvested capital and a strong demand among investors, which is likely to continue for years.
At the same time, for health systems, PE represents an important source of capital that can help fuel necessary growth. The key is to identify PE partners with deep healthcare expertise and a partnership orientation.
Through effective partnerships, where there is alignment between health systems, physicians and equity-backed platforms, all parties can realize benefits.
September 28, 2023
Written by Christian Lynch and Chance Sherer, CVA
Ambulatory surgery centers (ASCs) continue to be the target of health systems, physicians, and financial investors due to their straightforward business model and ability to align with physicians. As more high-acuity, high-reimbursing procedures transition to the outpatient setting, ASCs will become increasingly attractive for investment and will further cement their status as a preferred, low-cost surgical setting. Given the considerable attention from potential investors, it is crucial to understand how value is measured, how that value is derived, and the common terms used to describe value.
To convey value, market participants often speak in terms of “multiples.” A multiple is simply a company’s enterprise value divided by an industry-specific metric. Multiples are used due to their simplicity and ability to compare subjects to industry peers without the need for complex analyses. Although multiples within healthcare can be based on many different metrics, such as number of beds, revenue, covered lives, panel size, etc., ASCs are most discussed in terms of EBITDA multiples.
EBITDA, defined as earnings before interest, taxes, depreciation, and amortization, generally approximates a center’s cash flow, and by extension, its profitability. By calculating earnings before non-cash charges, such as depreciation and amortization, EBITDA represents earnings available to shareholders better than net income. Additionally, excluding interest expense removes the effect of capital decisions, whereby shareholders decide to finance purchases with debt or purchase equipment outright. Due to the discretionary nature of utilizing debt instead of cash, removing the impact of such decisions makes EBITDA an easily comparable metric between industry participants.
Understanding EBITDA and its benefits provides a clearer picture of multiples and their meaning. For example, a multiple of 8x EBITDA means the target ASC can be wholly acquired for a sum equal to eight times its EBITDA. Despite the prevalence and simplicity of EBITDA multiples, there are a few significant pitfalls to be aware of.
First, it is important to recognize that EBITDA multiples are often discussed in terms of “implied” multiples rather than “applied” multiples. Put another way, the final transaction value is typically determined through a detailed analysis of the subject ASC’s historical and projected financial performance. This value is then divided by EBITDA to arrive at an implied multiple.
Investors and valuation professionals are concerned about the ultimate distributions received from an investment in an ASC and the associated risk/return. The distributions are assessed through a discounted cash flow analysis where future earnings are projected and discounted back to present-day dollars using a discount factor. The sum of these discounted cash flows is then used to estimate the value. This analysis allows for the consideration of many idiosyncratic factors relevant to the subject ASC, such as size, geography, capacity, specialty/case mix, payor mix, staffing and supply expense growth, capital requirements, and many other factors.
Conversely, simply applying a market multiple to EBITDA will give an indication of value but may not accurately reflect the specific factors of the subject ASC. Given the intricate analysis used to determine value, it is clear why ASC transactions at the control level do not all occur at the same multiple; one center may be valued at a 7.3x implied EBITDA multiple, and another may be valued at an 8.2x multiple.
Buyers and sellers must understand the range of EBITDA multiples in the market to ensure the analysis produces an appropriate result. If the implied multiple lies outside the market range the discounted cash flow analysis will provide an explanation as to why.
To fully understand an implied EBITDA multiple is it critical to know the EBITDA by which the multiple is calculated. As shown in the table below, the implied EBITDA multiple of ASC value can be expressed using several different types of EBITDA; however, the most common are historical, normalized, and projected. Historical EBITDA represents the actual earnings of the center in the prior 12 months. On the other hand, normalized or adjusted EBITDA represents earnings after adjusting revenues and expenses to depict what a normal past 12 months of operations would have looked like.
Typical adjustments include the removal of one-time expenses and revenues, transaction adjustments for related-party arrangements (i.e., management agreements, billing fees, rent expenses), and adjustments for the timing of certain revenues and expenses that are over-represented or under-represented in the examined historical period. Lastly, projected EBITDA represents the expected next 12 months of earnings after normalization. It may account for many specific factors, but commonly it varies from normalized EBITDA due to expected changes in case volume.
Using different types of EBITDA can have a material effect on multiples. For example, after removing certain nonrecurring expenses, a center’s normalized EBITDA might be $100,000 higher than the historical level. As a result, a control-level value indication of $10,000,000 would produce a multiple of 8.3x based on historical EBITDA, whereas using normalized EBITDA would imply a multiple of 7.7x.
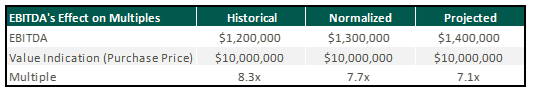
Though implied multiples are often discussed in terms of normalized or projected EBITDA, sellers should be cautious when hearing rumored valuation multiples among their peers. A possible disconnect between the various indications could distort the view of how ASCs are valued.
While it is beneficial to understand the general market ranges for ASC transaction multiples, an extensive assessment of the specific facts and circumstances of any singular center is required to determine its precise value. This valuation requires detailed knowledge of the operations and financial performance of the ASC from both a historical and future perspective. To determine an accurate valuation range for a center, buyers and sellers commonly engage the services of qualified advisors, such as VMG Health, who have extensive experience in ASC valuation.
September 21, 2023
Written by Josh Miner, Savanna Ganyard, CFA, and Taryn Nasr, ASA
The Ambulatory Surgery Center (ASC) market is a fast-growing sector of healthcare that is attracting considerable interest from private equity (PE) funds across the country. The following outlines the current state of the market as well as key factors driving ASC market growth and attracting PE investment.
2021 saw the most PE-related healthcare transactions in history, with an estimated 1,018 transactions occurring throughout the year. During the first quarter of 2023, transaction activity slowed from the pace set in 2021, primarily due to macroeconomic factors including inflationary pressures, rising interest rates, and higher labor costs. Additionally, rising interest rates and tight credit have increased the cost of debt leading to a reduction in leverage of one to one-and-a-half turns. Uncertainty surrounding the bank debt market has led PE investors to turn to private credit and other deal strategies. These strategies include searching for smaller deals where securing financing may be easier or targeting add-ons that are small enough to purchase without debt.
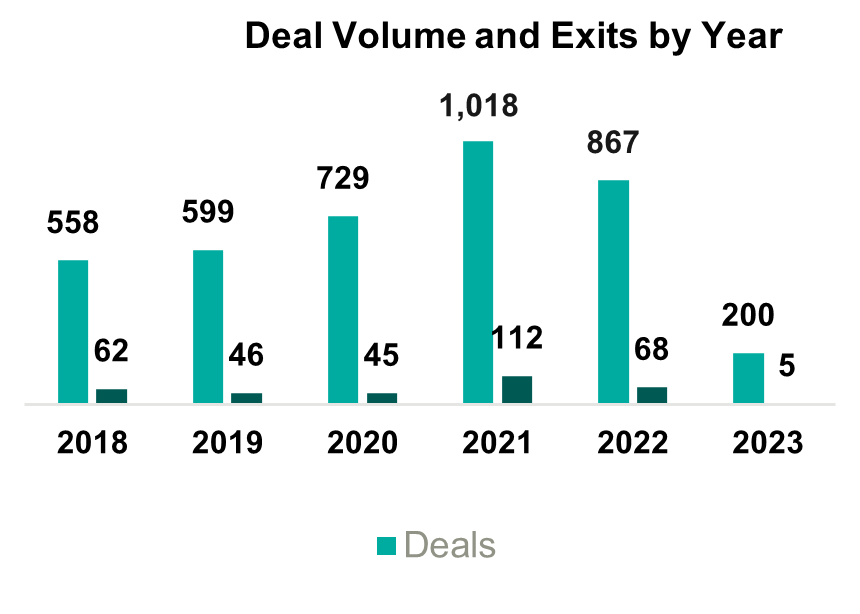
Despite the recent slowdown in activity, it is likely that the deal volume will rebound as macroeconomic uncertainty eases, but, in the short term, PE firms will likely continue to target smaller platform deals and add-ons. These transactions will likely involve independent targets, as other institutional investors may not attempt an exit in the current economic conditions.
The ASC market was recently sized at $84 billion in 2020 and is projected to grow at a compounded annual growth rate (CAGR) of 3.9% to $131 billion by 2031. The industry is highly fragmented with 70% of ASCs independently owned and the remaining owned by larger conglomerates. Over the past several years, PE ownership in the ASC space has steadily increased. Two of the largest players in the industry, AmSurg and Surgery Partners, have PE ownership. Other major ASCs with PE ownership include Covenant Physician Partners, EyeCare Partners, Gastro Health, GI Alliance, HOPCo, PE GI Solutions, and Value Health. Notably, Bain Capital’s $3 billion leveraged buy-out (LBO) of Surgery Partners in 2017 remains the largest deal completed in this space.
The expected growth in the ASC industry is driven by numerous factors including a shift towards lower cost procedures. On average, patients save $684 per procedure at an ASC as compared to a hospital based on a 2021 report from UnitedHealth Group. Specifically, orthopedics is a growth area driven by cost savings. On average, ASCs reduced the cost of orthopedic procedures by 17% to 43%. These cost savings at an ASC lessen the burden on the patient and help boost margins in an ASC setting. As a result, orthopedics continues to be a popular specialty for investors pursuing an ASC strategy.
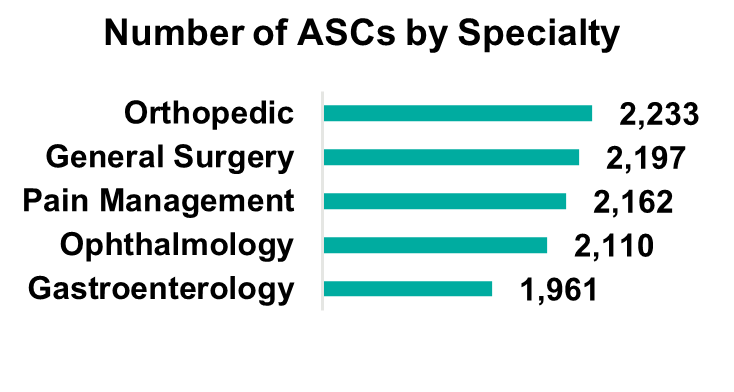
Orthopedics remains the most popular specialty, but gastroenterology, pain management, and ophthalmology make up large portions of the market. Notably, cardiology has become the fastest-growing specialty as ASCs invest in technology and higher acuity procedures continue to move to the ASC setting. The demand for cardiology is driven by an aging population and the level of cardiovascular disease in U.S. adults (e.g., half of all U.S. adults have cardiovascular disease). While cardiology is currently primarily a hospital-based specialty, with 70% of cardiologists employed by hospitals, as this specialty moves into ASCs there is a unique opportunity for PE firms to secure a foothold in a fast-growing segment.
On January 31, 2023, Lee Equity Partners (LEP) completed a buyout of the Cardiovascular Institute of the South (CIS) for an undisclosed amount (of note, LEP deals typically range from $50 to $150 million in equity). CIS has 21 locations across two states and employs over 60 physicians. This deal represents one of the larger buyouts of an ASC in recent memory and illustrates the growth of cardiology as a specialty in ASCs.
As more cases and specialties shift to an ASC setting, there is an increasing patient demand for multi-specialty ASCs. Patients are seeking convenience in the ability to receive treatment for a multitude of treatments in one place. The number of multispecialty ASCs is forecasted to expand at a 4.3% CAGR, outpacing general ASC market growth.
These industry characteristics coupled with the PE industry outlook should continue to drive transactions within this space, specifically among the 70% of independently owned ASCs. Due to recent macroeconomic factors, we expect PE firms to continue to pursue smaller add-on deals aimed at consolidating several ASCs in an area. These types of transactions allow PE firms to capitalize on industry trends, optimize cost-cutting opportunities, and generate attractive returns. On the other hand, these transactions are also attractive to independent and physician-owned ASCs due to the benefits of a larger growth infrastructure which can leave more time for physician owners to focus on patient care.
ASCs can offer cost savings and convenience to consumers without sacrificing quality of care. Due to increasing demand, the number of specialties, and the ability to perform high-acuity procedures, the ASC market is projected to grow steadily over the next decade. Market growth, combined with the availability of investment opportunities due to the fragmentation of the market, will continue to attract PE investment. As macroeconomic conditions become less uncertain, it is likely that PE investment will continue to rebound to historical levels in the healthcare industry. Furthermore, the many attractive qualities of the ASC industry should draw investment in the space.
September 14, 2023
Written by Anthony Domanico, CVA and Ben Minnis, CVA
The following article was published by the American Association of Provider Compensation Professionals.
In the rapidly evolving landscape of healthcare, traditional fee-for-service (FFS) reimbursement models are being replaced by alternative payment models that focus on value-based care in addition to, or even sometimes fully in replacement of, fee-for-service reimbursement. This shift from volume to value necessitates a strategic rethinking of compensation plans for healthcare providers to align incentives, optimize patient outcomes, and maximize revenue. The implementation of value-based compensation plans requires a deep understanding of the intricacies of different alternative payment models and the development of innovative strategies to ensure financial success while prioritizing quality care.
A key tenet of value-based care is the focus on delivering high-quality healthcare outcomes to patients while managing costs effectively. Alternative payment models, such as bundled payments, accountable care organizations (ACOs), and capitation, incentivize providers to prioritize preventive care, care coordination, and patient engagement while reducing unnecessary or inappropriate services.
These models differ from traditional fee-for-service, which rewards the quantity of services delivered rather than their outcomes. Under a fee-for-service reimbursement model, the more you do, the more you get. This is the case even if certain types of care or services are not warranted, are considered excessive based on the problem set presented by a particular patient, or do not lead to good patient outcomes.
However, under value-based contracts providers are rewarded not for the volume of services rendered, but for providing high-quality care to a large population of patients while also reducing unnecessary and/or inappropriate services.
While all value-based care models pay for value in some respect, the way various payment programs are structured will determine what compensation mechanism(s) will lead to better outcomes for both the physician and the organization.
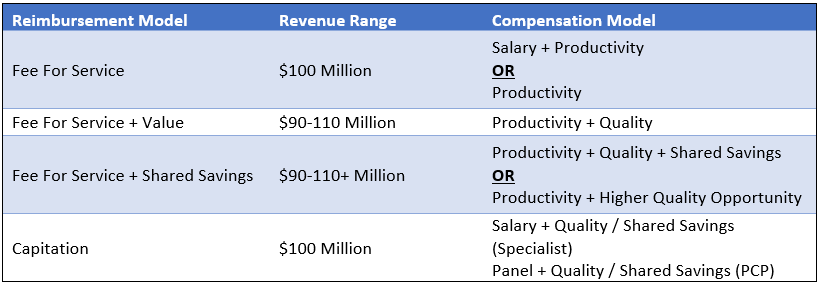
Consider the following scenarios that are all focused on a hypothetical organization with $100 million of revenue and 200 FTE doctors ($500,000 in revenue per FTE).
Under a non-capitated value-based model where the organization continues to earn reimbursement under an FFS construct, with additional revenue opportunities through quality incentives, that organization might see $90 million of FFS revenue for the same book of business. In addition, that organization can earn up to an additional $20 million in value-based payments for a total possible range of $90-110 million of revenue.
Under this reimbursement structure, the organization will still be incentivized to have its physicians rewarded for productivity. After all, a sizable portion of the organization’s revenue, and most of the organization’s ability to increase the revenue pool (the $90 million), is through FFS reimbursement. As such, a compensation model under this construct might be a productivity model (with or without a base salary component). Also, it would include an additional incentive opportunity for value-based arrangements based on the metrics included in the organization’s value-based contracts.
Another emerging component of value-based contracts is shared savings opportunities. If an insurer typically incurs costs of $10 million for managing a population of patients, and the subject organization can take high-quality care of the same population of patients for $9 million, insurers are increasingly sharing a portion of the cost savings back to the providers/health systems that are helping to achieve these savings.
Designing compensation arrangements to maximize shared savings opportunities is much trickier than under FFS and value models. After all, it is much more challenging to define metrics around achieving cost savings on a targeted population of patients than it is to measure things like hemoglobin A1c scores. As a result, we often see organizations either use shared savings dollars earned from insurers to fund larger quality incentives or pass through a portion of those earned dollars received from insurers to network physicians.
The latter option is complex in that it requires organizations to understand how those cost savings are achieved and to be able to allocate those savings earned down to the individual physician level or develop a proxy formula to estimate these factors for payment. As an example, we may see an organization decide to withhold 50% of funds earned to cover the additional costs incurred by the employer (such as hiring care coordinators to ensure patients with diabetes are getting back to the clinic for follow-up tests, etc.), and distribute the remainder by using a formula based on quality, wRVUs, or some other distribution formula.
Ensuring compensation remains consistent with fair market value under these types of arrangements is challenging. With that in mind, you will want to ensure you are working with counsel and a compensation design/valuation expert to ensure any compensation models remain consistent with fair market value.
At the other end of the volume-to-value spectrum are capitation models which include an organization that receives a fixed payment on a per member per month basis for all members under its care. Under these models, if those 200 FTE physicians manage a panel of 50,000 patients, and the organization is reimbursed $166.67 per patient per month, that organization receives a total annual payment of $100 million.
Under these models, the organization receives a fixed payment regardless of its costs, assuming it has the same number of patients. An organization can only increase top-line revenue through growth in the patient population served, so compensation models tend to be a combination of fixed and variable. Specialists might be paid on a salary-type model (with or without incentives), while primary care providers might be paid on an acuity-adjusted panel size model whereby physicians are incentivized to take on more patients and grow the total capitated revenue of the organization.
These models may also include incentive payments tied to care coordination, quality outcomes, cost controls/reductions of unnecessary or inappropriate services, and the like.
The table below summarizes the options discussed. Note that the compensation models in the right-hand column are the most predominant compensation model structures for a particular reimbursement model. However, other models may be more appropriate depending on the facts and circumstances impacting the subject organization.
In addition to designing compensation models that allow for maximum revenue potential, organizations must enact robust change management processes to ensure their providers are not lost in the transition to a new compensation model. Providers need to understand the rationale behind the new models and how their efforts contribute to both patient care and financial success for the organization and the providers. Regular feedback loops and performance evaluations can help providers track their progress and make necessary adjustments.
As healthcare continues to shift toward value-based care, designing an effective compensation plan is becoming increasingly crucial for provider organizations to thrive under these alternative payment models. The suitable model for your organization might vary significantly from the compensation structure observed at the neighboring health system. This is especially true considering both organizations could be positioned at distinct points along the risk continuum.
The key success driver is for organizations to design models that will help them be successful wherever they are on the continuum. By aligning incentives with patient outcomes, leveraging innovative strategies to provide more cost-effective care, and adapting to changing market dynamics, organizations can optimize revenue and physician-earning opportunities while delivering high-quality care to their patients.
September 6, 2023
Written by Nick Shannon, ASA, and Joel Gomez, ASA
Earlier this year, the United States Attorney’s Office Eastern District of Michigan issued a press release regarding a False Claims Act settlement involving a regional hospital system and physicians. Specifically, Covenant Healthcare System paid $69.0 million to settle allegations in 2021 under the False Claims Act related to improper financial relationships with eight physicians and a physician-owned investment group. In addition to the False Claims Act, there were specific allegations pertaining to the Anti-Kickback Statute (AKS) and The Physician Self-Referral Law (Stark Law).
One component of the allegations included a medical equipment lease arrangement between Covenant and the physician-owned investment group. It was alleged that Covenant permitted the group to structure the equipment lease under non-arms-length negotiations with the purpose of inducing patient referrals.
Many health systems and physicians/physician groups pursue lease arrangements to provide flexibility in assessing long-term relationships and to reduce capital expenditure at the outset of an employment agreement. These agreements may include traditional personal property fixed asset leases, such as furniture, fixtures, and equipment, or material capital asset leases such as major movable medical equipment. With the increased popularity and projected growth of medical equipment lease agreements, there is the possibility of increased scrutiny and consideration of whether these agreements comply with federal laws.
The structure of the equipment lease transaction has a significant impact on fair market value requirements, as well as other tax, accounting, and financial reporting requirements. When planning an equipment lease arrangement all parties involved should consider the following:
For federal income tax purposes, the Internal Revenue Service (IRS) has established guidelines for “true leases” or “fair market value lease.” This guidance specifies that a true lease, or operating lease, involves a lease transaction where the lessor is deemed the owner of the asset and receives all depreciation and tax benefits. Guidelines to consider for true lease classification include:
If the above guidelines are not satisfied, a lease transaction would be considered a non-tax lease, or capital lease, where depreciation and tax benefits fall with the lessee.
Another consideration, for both a potential lessor and lessee, is to evaluate the accounting treatment and impact for a particular classification of the lease. For example, a potential lessee interested in reporting a capital lease for financial reporting purposes would need to confirm at least one of the following criteria:
Alternatively, if the potential lessee cannot confirm any of the above criteria, they would classify the lease as an operating lease.
Once the appropriate equipment lease structure is determined the underlying details of the arrangement should be evaluated considering Stark and AKS, assuming the potential for financial and referral relationships between the parties.
Under Stark Law Section 42 CFR § 411.357(b) exceptions to the referral prohibition related to compensation arrangements subset (b) Rental of Equipment states that equipment lease arrangements do not constitute a financial relationship if the payments made by a lessee to a lessor meet the following requirements:
Similarly, AKS Section 42 CFR § 1001.952(c) outlines safe harbor related to equipment rental by meeting the following six standards:
In summary, the absence of arms-length negotiations could imply equipment lease payments constructed above or below fair market value, and therefore, not meeting Stark exception requirements under Rental of Equipment that states, “The rental charges over the term of the agreement are consistent with fair market value.”
Stark Law defines fair market value, with respect to the rental of equipment, as “the value in an arms-length transaction of rental property for general commercial purposes, consistent with general market value.”
In addition, AKS prohibits soliciting or receiving remuneration “in return for purchasing, leasing, ordering, or arranging for or recommending purchasing, leasing, or ordering any good, facility, service, or item for which payment may be made in whole or in part under a federal healthcare program.”
August 28, 2023
Written by James Tekippe, CFA, Michael Schenck, and Ryan Diver
The following article was published by Becker’s ASC Review.
The No Surprises Act was a landmark piece of legislation aimed at protecting patients from unexpected medical bills. Although the law is a significant step forward for patient protection, it has resulted in a significant increase in financial support requests from anesthesia providers who serve patients at ambulatory surgery centers (ASCs). This article will outline the hallmarks of the act, its impact, and the operational and compliance considerations for ASCs that need to implement coverage arrangements with their anesthesia groups.
Prior to the No Surprises Act, patients who unintentionally received care from an out-of-network provider could potentially have received a “surprise medical bill” from a facility or provider. This occurred in emergency room situations where the patient had no ability to select the emergency room, physician, or ambulance provider. Additionally, surprise bills resulted from services provided at an in-network facility for a patient but from an out-of-network provider. This was common for services provided by anesthesia, first assist, and radiology providers.
Additionally, healthcare costs and pricing information were often difficult to obtain prior to receiving treatment, and patients frequently faced challenges in understanding the cost implications of their healthcare choices. Moreover, billing disputes between healthcare providers and insurance companies often left patients caught in the middle. Consequently, surprise medical bills could result in higher fees for patients in a couple of ways. First, higher cost sharing between health plans and patients, with most patients having to pay a higher co-pay for out-of-network services. Second, many providers would balance bills, which allowed “the out-of-network provider [to] bill consumers for the difference between the charges the provider billed, and the amount paid by the consumer’s health plan.”
Due to these circumstances, the No Surprises Act was passed as part of the Consolidated Appropriations Act, 2021 and began taking effect on January 1, 2022. Now after a patient receives care, the healthcare provider will verify the patient’s insurance and determine if they are in-network or out-of-network. If the patient receives care from an out-of-network provider at an in-network facility, the patient is only responsible for their in-network cost-sharing amount, such as deductibles, co-pays, or coinsurance. The provider will then bill the insurance for their services. After the insurance company processes the provider’s claim, the patient will then be billed for their responsibility for the in-network cost-sharing amounts. If there is a dispute between the provider and the insurance company regarding reimbursement for out-of-network services, the provider and insurance company may engage in the independent dispute resolution (IDR) process, where an independent arbiter reviews the case and determines the appropriate payment.
The implementation of the act has caused tension between providers and insurers. Prior to the act, many providers had relied on balance billing to generate revenue. Now, not only is this practice illegal in certain scenarios, but insurance companies are typically only willing to pay something near the qualified payment amount (QPA), which is the median rate for those in-network services for the given geographical area. This can neglect crucial factors and can be very different from the amount they were used to receiving. This has resulted in numerous providers and payers entering negotiations and the IDR process.
Given the reduction in billings that some provider groups may be experiencing because of the No Surprises Act, anesthesia groups with coverage arrangements with ASCs have found themselves requesting additional compensation. For some ASCs, this is a request they are grappling with for the first time. It is very important to understand that these arrangements are set at fair market value from a compliance perspective. To help navigate these arrangements, VMG Health has outlined some important factors for ASCs to consider.
When establishing an arrangement for coverage to be supplied by an anesthesia group, it is important for ASCs to understand what level of coverage they will need. This includes a consideration of on-site time needed versus off-site or on-call time. Additionally, it is important to establish the need for medical directorship or other administrative services with a provider group, including an expectation of hours for these roles.
Facilities should consider what types of providers are needed and should confirm with the provider group that this level can be supplied. Leaning on certified registered nurse anesthetists (CRNAs) can be beneficial from a cost perspective for both the provider group and the facility, but the facility should ensure the mix is appropriate for the coverage needed. As provider compensation is typically the largest expense driver in coverage arrangements, it is, of course, important to ensure the right level of expertise is provided. However, the ability to lower provider expenses by leaning on CRNAs should not be overlooked.
As the industry continues to shift towards value-based care, certain quality incentives may be considered for inclusion in a coverage arrangement. Facilities contemplating adding these types of metrics should push for outcomes-based metrics that the providers will have the ability to demonstrably impact. Additionally, facilities should ensure that accurate tracking of outcomes is possible and that targets require the attainment of higher quality versus maintenance of current outcome achievements.
To service a coverage arrangement, provider groups typically will need to incur some additional costs beyond provider comp expenses, including billing and collection expenses and general office support expenses. However, additional requirements might be needed from a facility. Therefore, facilities should work with groups to outline their needs to ensure the provider group is aligned with the expectations under the arrangement beyond the clinical provider requirements.
The No Surprises Act is a major step towards protecting patients from unexpected medical bills, but it presents significant challenges for healthcare providers. Providers must adapt to the new law’s requirements, which can be time-consuming, costly, and complicated. While providers will need to be proactive in addressing these challenges, facilities may be asked to provide further financial assistance in certain arrangements. Having open and thorough conversations about the needs of the facility, while balancing the challenges faced by anesthesia groups, will be an effective way for facilities and providers to continue partnering to provide high-quality care for patients.
August 7, 2023
By Anthony Domanico, CVA, and Ben Minnis
VMG Health was published in the American Association of Provider Compensation Professionals (AAPCP) 2023 Journal of Provider Compensation. The section, “How to Measure Acuity-Adjusted Panel Size for Contemporary Provider Compensation Plans” was written by VMG Health experts Anthony Domanico and Ben Minnis.
In their section, Domanico and Minnis offer a detailed examination of diverse panel size approaches and important factors to consider when incorporating these metrics into a compensation plan. As organizations take on greater financial responsibilities in payer agreements, it is vital to ensure that incentives harmonize with compensation plans.
The second edition of this journal provides an in-depth analysis of issues such as financial pressures medical groups are facing, optimal timing for adopting a new Medicare Physician Fee Schedule, whether wRVU-based compensation plans remain the guiding principle for employment arrangements, and concerns about the emerging physician shortage. The five articles published in this edition all passed through a rigorous framework to ensure quality analysis.
For additional guidance related to provider compensation design or any other valuation, strategy, or compliance services, our expert Anthony Domanico would be happy to assist. Please email him at anthony.domanico@vmghealth.com to learn more.
August 7, 2023
By James Tekippe, CFA – VMG Health, and Courtney Stokes, JD, MHSA – Kathleen L. DeBruhl & Associates, LLC
The following article was published in the American Bar Association Health Law Section’s eSource.
Prior to the onset of the COVID-19 pandemic, the issue of career fatigue was already a growing concern for physicians and healthcare systems. In 2018, a survey conducted by The Physicians Foundation reported that 31% of physicians indicated they often have feelings of burnout. Fast forward a few years into the pandemic, and in the 2022 edition of this survey, this number has jumped to 62% of respondents indicating that they often have feelings of burnout. This growth in burnout is a major concern as physician burnout negatively impacts physicians’ well-being, decreases the quality of care physicians provide, and contributes to older physicians retiring earlier than anticipated and younger physicians leaving the field altogether. While many of the reasons for these results were present before COVID-19, the pandemic has brought this discussion into new context and importance.
This is the first in a three-part series on physician career fatigue and mental health issues. This article will examine four of the major causes of career fatigue for physicians: administrative burdens, including those created by the advent of electronic health records (EHRs), the increase in violence in the healthcare setting, the continued industry-wide staffing shortages, and the persisting stigma associated with seeking treatment for a mental health condition or substance use disorder. While there are no simple answers or quick fixes for these issues, this article will include a discussion of potential solutions that various stakeholders around the country are adopting in an attempt to positively address physician career fatigue and burnout.