- About Us
- Our Clients
- Services
- Insights
- Healthcare Sectors
- Ambulatory Surgery Centers
- Behavioral Health
- Dialysis
- Hospital-Based Medicine
- Hospitals
- Imaging & Radiology
- Laboratories
- Medical Device & Life Sciences
- Medical Transport
- Oncology
- Pharmacy
- Physician Practices
- Post-Acute Care
- Risk-Bearing Organizations & Health Plans
- Telehealth & Healthcare IT
- Urgent Care & Free Standing EDs
- Careers
- Contact Us
Behavioral Health Industry: Impact of COVID-19
April 29, 2020
Written by Clinton Flume, Kelly Titus and Patrick Speights
Mental illness and substance use disorders (SUDs) are behavioral health conditions that affect millions of Americans. Every year, approximately one in five adults in the United States (47 million) experience mental illness. More than one-third of Americans (36%) say that COVID-19 is having a serious impact on their mental health.[i] In a recent survey conducted by the American Psychiatric Association, 19% of respondents reported having trouble sleeping, 8% reported having consumed more alcohol or other drugs, 12% reported that they have been fighting more with a partner or loved one, and nearly 1 in 4 people (24%) reported that they have been having trouble concentrating in their day-to-day lives due to thoughts about COVID-19.
Countless factors can contribute to the stressors that are experienced during a pandemic. As the number of unemployed individuals in the U.S. has risen from 6 million in January 2020 to 30 million in April, financial wellbeing is one of them. Other day-to-day stressors include the scarcity of essential items, such as food and medical supplies, social distancing guidelines, departure from routines, and changes in work habits. More long-term fears center around the lasting impacts the pandemic will have on the economy, people’s personal financial health, lifestyle changes, and a resurgence of the virus.
During this time of uncertainty, it is likely that mental health issues and substance use disorders among people with these conditions will increase. It is well-documented that the behavioral health industry is already saddled with a shortage of access to care and qualified professionals; thus, the remedies required to improve and support the industry will go far beyond the current short-term financial and regulatory relief introduced by the Trump administration in response to COVID-19.
In a letter sent to congressional leadership on April 29, 2020, a bi-partisan group of lawmakers, in support of the American Society of Addition Medicine (ASAM) and the National Counsel for Behavioral Health, advocated for emergency funding of $38.5 billion for behavioral health organizations (BHOs). According to the letter, BHOs have not received enough funding in the four stimulus packages to address the COVID-19 crisis. The emergency funding was requested to supplement projected BHO revenue lost in 2020, to aid Medicaid and the underserved population, to cover increased staffing costs and PPE, and to increase investments in telehealth[ii] [iii].
Along with the Trump administration’s current behavioral health aid to counter the pandemic, including CAREs Act funding and waived regulations and restrictions, industry stakeholders require further resources to combat COVID-19’s impact.
CARES Act Impact on the Behavioral Health Industry
On March 27, 2020, the Coronavirus Aid, Relief and Economic Security (CARES) Act was signed into law. It provided a total of $2.3 trillion in stimulus with funding for loans to businesses, direct relief to individuals in the form of payments and unemployment benefits, numerous supports for other programs, and approximately $180 billion in healthcare-specific funding.
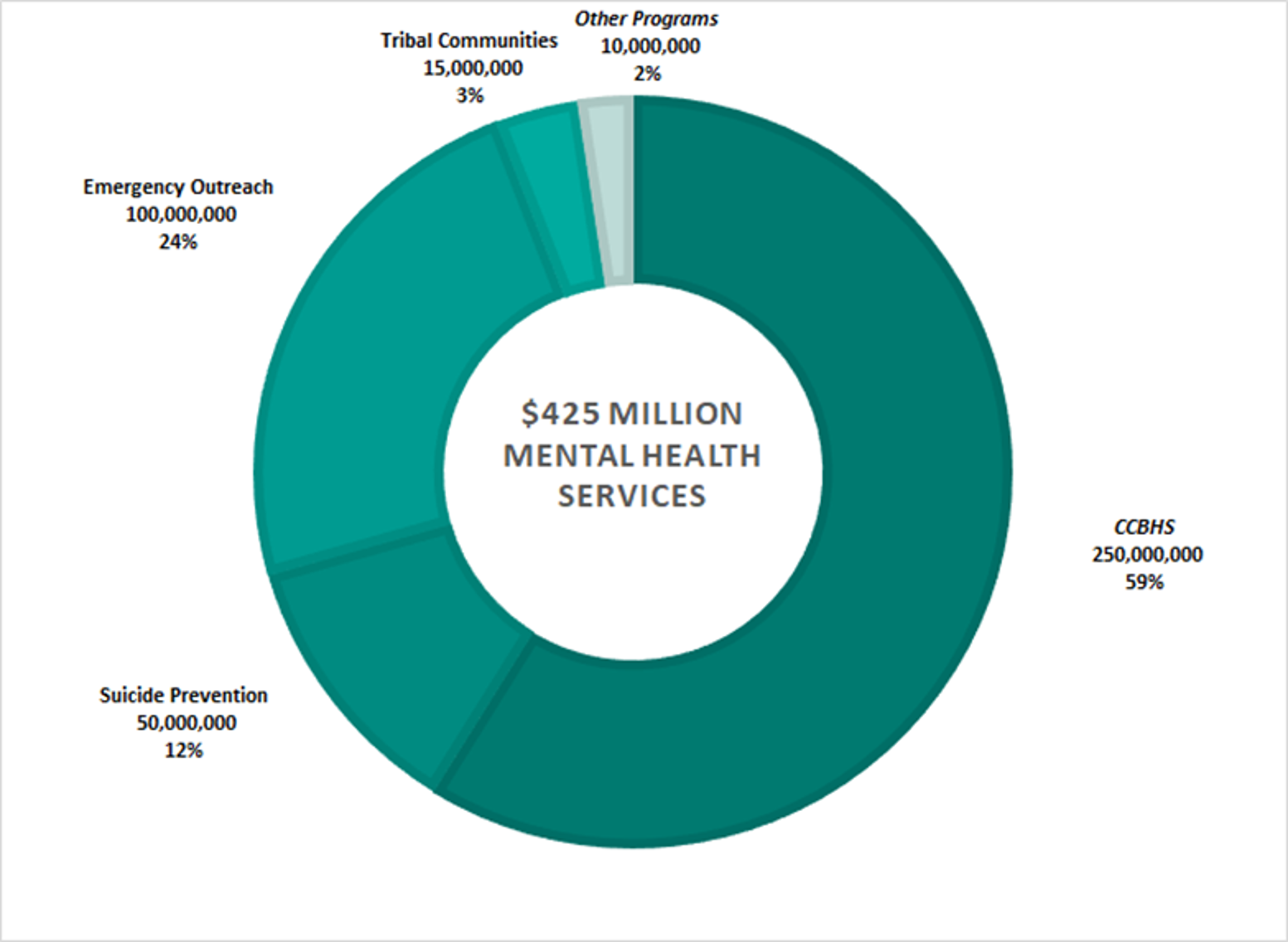
Of the $180 billion in healthcare funding, approximately $425 million was allocated to the Substance Abuse and Mental Health Services Administration (SAMHSA), with the greatest allocation made to Certified Community Based Health Services (CCBHS).[iv] The complete allocation of these funds is detailed below.
Additionally, $29 million was allocated to the Telehealth Network and Telehealth Resource Centers Grant Programs for fiscal years 2021–2025. Temporary relief for telehealth and high deductible health plans was provided, allowing coverage for telehealth services without plan member costs before plan members’ deductibles are met.iv According to the ASAM, the added benefits of telehealth include the continued promotion and practice of social distancing and the allowance of healthcare professionals to monitor and administer treatment in safe settings.[v] The importance of continued support for telehealth resources will positively impact the behavioral health community and help reduce the barrier of access to services and qualified professionals.
Section 1135 Waiver
The Trump administration made regulatory changes to the U.S. healthcare system as part of the ongoing White House Coronavirus Task Force efforts. Many restrictions have been relaxed to help relieve the burden from healthcare providers to allow them to continue providing quality care to patients.
- As part of the Section 1135 waiver authority, CMS has waived Medicare and Medicaid requirements that practitioners be licensed in the state in which they are furnishing their services.
- Section 1135 has expanded telehealth services by 80 current procedural terminology codes. Providers can bill for visits at the same rate as in-person visits. Providers can conduct virtual face-to-face visits required in inpatient rehabilitation facilities, as well as virtual staff supervision. As of April 23, 2020, 47 states have relaxed their state licensure restrictions regarding telehealth.
- CMS is allowing hospitals to transfer non-COVID-19 patients to inpatient rehabilitation hospitals, hotels, and dormitories to make room for infected patients. Hospitals can use acute care beds for psychiatric needs so long as they have a separate, distinct inpatient rehabilitation unit.
- CMS has allowed a critical access hospital to admit in excess of 25 patients and to maintain individuals as inpatients for more than 96 hours.
- DEA-registered practitioners may prescribe controlled substances through telehealth for new patients without having an in-person evaluation.
(vi, vii, viii)
Substance Use Disorders
On March 16 and again on March 19, the Department of Health and Human Service’s Substance Abuse and Mental Health Administration (SAMHSA) issued FAQs that highlight the provisions being made for COVID-19. ix These include the provision that practitioners working in an Opioid Treatment Program (OTP) or Office-Based Opioid Treatment program can prescribe buprenorphine for new patients, utilizing telemedicine instead of requiring an in-person visit. SAMHSA is also allowing states to request blanket exceptions for all stable SUD patients in OTPs to receive extended prescriptions of take-home medications for treating their addictions.x
A substantial part of the protocol for substance abuse treatment is gathering and incorporating accurate lab results into treatment planning. While the option to conduct examinations via telehealth is an excellent alternative for both patient and practitioner, telehealth does not address the need for gathering and completing lab work. Thus, the logistics challenges surrounding the lab component remain, presenting significant financial challenges for providers.
For Americans who struggle with SUDs, waiver restrictions supporting telehealth visits can provide the continuity of care SUD patients require to develop a long-term plan for addiction management.
VMG Health Commentary
The COVID-19 pandemic has put the American healthcare system into an era of introspection whereby federal and state officials, along with healthcare executives and frontline workers, are forced to manage these unprecedented challenges. For those Americans who faced mental health illnesses or SUDs pre-COVID-19, these health issues will long persist post-quarantine and stay-at-home orders. Those who did not previously shown signs of depression, anxiety, or substance abuse may be at a heightened risk for developing these tendencies in this new COVID-19 environment. The behavioral health industry has received reprieve through the CAREs Act, reduced regulation through CMS’ blanket waivers, and other state and local regulations. In the short term, the behavioral health industry is unlikely to remedy the scarcity of qualified professional providers or allow adequate access to inpatient and outpatient services As the market moves forward, a renewed focus on addressing funding shortfalls, market reimbursement alignment, greater access for participant coverage, and acknowledgment of the role that mental health and SUDs play in our everyday lives will be required for the industry to leverage and accelerate this movement.
i https://www.psychiatry.org/newsroom/news-releases/new-poll-covid-19-impacting-mental-well-being-americans-feeling-anxious-especially-for-loved-ones-older-adults-are-less-anxious
iihttps://www.warren.senate.gov/imo/media/doc/2020.04.29%20Letter%20to%20Congressional
%20leadership%20re%20mental%20health%20emergency%20funding.pdf
v https://www.asam.org/Quality-Science/covid-19-coronavirus/access-to-telehealth
ix https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
x https://www.samhsa.gov/sites/default/files/otp-guidance-20200316.pdf
Categories:
Subscribe
to our blog