- About Us
- Our Clients
- Services
- Insights
- Healthcare Sectors
- Ambulatory Surgery Centers
- Behavioral Health
- Dialysis
- Hospital-Based Medicine
- Hospitals
- Imaging & Radiology
- Laboratories
- Medical Device & Life Sciences
- Medical Transport
- Oncology
- Pharmacy
- Physician Practices
- Post-Acute Care
- Risk-Bearing Organizations & Health Plans
- Telehealth & Healthcare IT
- Urgent Care & Free Standing EDs
- Careers
- Contact Us
CMS Proposed Changes to 2013 Physician Fee Schedule
August 2, 2012
The Center for Medicare and Medicaid Services (CMS) released its’ proposed rule (Rule) for changes related to payment policies under the physician fee schedule and other areas on July 6, 2012. According to a copy of the Rule on the Office of Federal Register website, the Rule “…addresses changes to the physician fee schedule, payments for Part B drugs, and other Medicare Part B payment policies to ensure that our payment systems are updated to reflect changes in medical practice and the relative value of services.” As is its’ custom, comments on the Rule may be submitted for a 60 day period after the initial date of filing for public inspection.
Likely considered the most significant change is the projected 27 percent cut in Medicare payment rates as suggested by the sustainable growth rate (SGR) formula. However, there are indications that Congress may be acting to delay this projected cut. Representative Michael Burgess (R – TX) has said he will submit legislation that would delay the SGR cuts for one year. If historical precedent is any indication, some sort of delay related to the SGR cuts is highly likely.
There is an emphasis on primary care in the Rule; likely a result of healthcare reform and the focus on patient care coordination. For family physicians, the Rule proposes a 7 percent increase in payments while other primary care practitioners would receive a 3 – 5 percent increase. While primary care providers will see increases, the Rule includes payment cuts to several specialty groups. The specialties or areas with the largest proposed cuts – on top of the proposed SGR reduction – are summarized in the chart below:
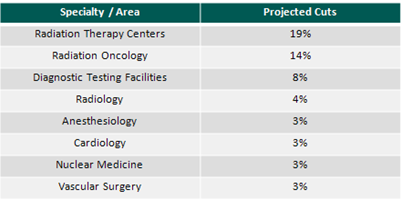
Much of the proposed decline in imaging services is related to a reduction in payment when more than one imaging service is provided by the same physician(s) to the same patient, during the same session (visit), on the same day. This is simply an expansion of the multiple procedure payment reduction (MPPR) often utilized by Medicare. In such cases, the lower priced procedure would receive a 25 percent reduction in payment. Specifically for radiation oncology, payment cuts surround two services: intensity modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT). In both cases, CMS has reviewed the clinical times that were initially utilized to determine reimbursement for these services and has concluded that the times are too high based on current information. Also driving this reduction is a change in the interest rate assumption used to determine the payment component for practice expenses. The interest rate change would decline from 11 percent to a range of 5.5 – 8 percent which would impact services that require significant capital. The final rule is expected to be released on or around November 1.
Categories:
Subscribe
to our blog
