
CY 2022 Medicare OPPS and ASC Payment System Final Rule
Zach
November 17, 2021
Effective January 16, 2024, Compliance Risk Analyzer has joined VMG Health. Learn more.
November 16, 2021
Last year, the Centers for Medicare & Medicaid Services (“CMS”) revised the relative value units (“RVUs”) for many outpatient codes, specifically those related to evaluation & management (“E&M”). The Impact of the 2021 Medicare Physician Fee Schedule on Physician Practice Revenue and Provider Compensation provides an in-depth overview of the reimbursement methodology under the Medicare Physician Fee Schedule (“MPFS”) and the estimated impact on work RVUs (“WRVUs”) and Medicare reimbursement under the CY 2021 MPFS Final Rule. The 2022 CMS Physician Fee Schedule Final Rule (“CY 2022 Final Rule”) will implement less volatile, but important reimbursement changes beginning in January 2022.
Under the CY 2022 Final Rule, CMS finalized a reduction in the physician fee schedule conversion factor of 3.75% by decreasing the conversion factor from $34.89 to $33.59. The conversion factor reduction primarily reflects the expiration of the Consolidated Appropriations Act (“CAA”). The CAA was enacted by Congress in CY 2021 in response to the COVID-19 emergency, which temporarily provided a 3.75% increase in payments under the physician fee schedule for 2021, or about $3 billion in increased payments for physician services. With the CAA provisions expiring beginning CY 2022, CMS has finalized the reduction in the CY 2022 Final Rule, leaving many considering the material implications related to provider operations.
Understanding these changes is critical to proper financial planning and to appropriately assessing physician compensation. As healthcare leaders know, properly compensating physicians is key to alignment, care coordination and compliance. The following sections briefly describe the key changes outlined in the CY 2022 Final Rule and how to tackle existing and prospective physician compensation agreements under the new reimbursement environment.
In isolation, the theoretical effect to provider reimbursement due to the conversion factor adjustment will result in a 3.75% decrease in revenue for multi-specialty groups. In combination with other looming factors, providers are potentially facing up to a 10% cut to Medicare reimbursement beginning CY 2022. According to the American Medical Group Association (“AMGA”), providers are also facing a 2% Medicare sequester and a 4% Medicare cut due to Pay-As-You-Go (“PAYGO”) offsets required by the 2021 COVID-19 relief package.[1] Barring significant policy intervention, healthcare systems are facing drastic changes in reimbursement, which may, in turn, exacerbate provider shortages in an already overwhelmed space.
VMG has analyzed the expected changes detailed in the CY 2022 Final Rule. The table below summarizes VMG’s analysis on the estimated impact of the 2022 finalized changes to overall WRVUs and reimbursement for key medical and surgical specialties from 2020 levels.
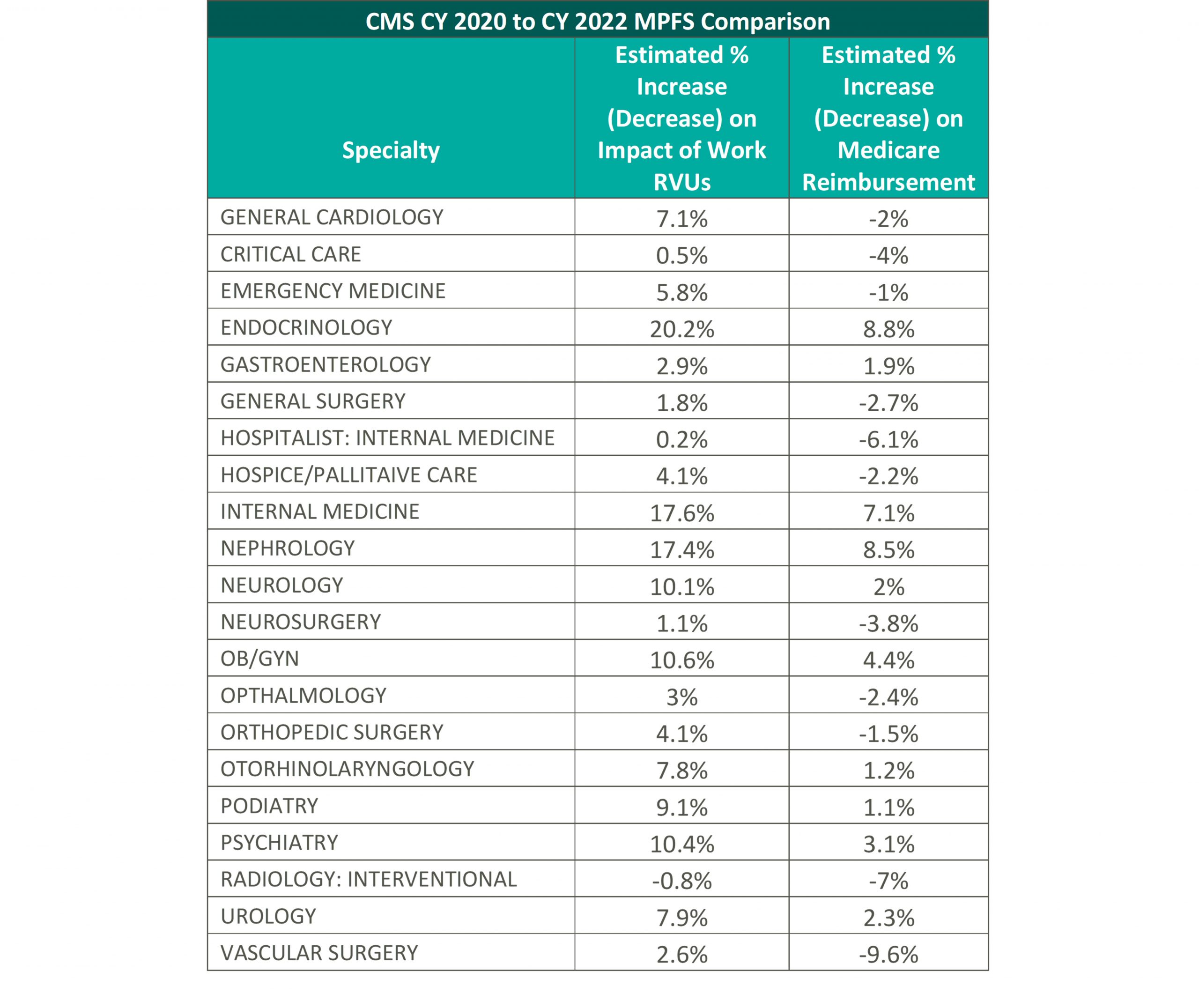
VMG has conducted an internal analysis for each specialty using 2022 RVUs and the 2022 conversion factor compared to the 2020 MPFS RVU factors (please see the above table for more detail) to determine the anticipated effects of the implementation of the CY 2022 Final Rule. Please note, VMG recognizes that the impact to individual practices and medical groups is heavily dependent on a provider’s service mix and the values reported in the physician fee schedule.
In consideration of the aforementioned changes, VMG believes it is crucial that healthcare systems who are currently utilizing the 2020 physician fee schedule consider the material impact in their operations that the CY 2021 and CY 2022 Final Rule may create. These considerations will be discussed in later sections.
The impact of the CY 2022 Final Rule has been heavily criticized thus far, as CMS received many comments of concern from healthcare associations to specialty physicians that are requesting CMS and other regulatory bodies to step in to prevent the decrease to the conversion factor. However, CMS has cited that because the initial increase was provided through a time-limited amendment to the statute (the CAA), CMS does not have legal authority to alter and, therefore, CMS cannot implement any long-term changes without guidance from regulatory bodies.[2] Below are a small sample of reactions from various physician organizations related to the CY 2022 Final Rule:
“Now that the decrease in the conversion factor is official, AMGA members need Congress to recognize the gravity of the situation. The decrease in the Medicare conversion factor, along with the looming sequester and PAYGO cuts, will undermine the ability of AMGA members to care for their patients. Failing to prevent these cuts could result in significant challenges. Our members will need to make hard choices, and will need to consider hiring freezes and layoffs, as well as service line eliminations. It’s a critical situation, and Congress needs to treat it as such.”[3] [American Medical Group Association]
“Surgeons and their patients have already been significantly impacted by the pandemic. These Medicare cuts will further exacerbate our pandemic-strained health care system and cause further delay in care to the patients who need it most.”[4] [American College of Surgeons]
“We are once again facing a potential drastic cut in physician payments at the end of the year. It is imperative that Congress step in to prevent the cuts and ensure stability while our health care system is still in the midst of the COVID-19 pandemic. The impact to physician practices will be even greater when you couple these cuts with the huge impact that the pandemic has had on internal medicine specialists and other frontline physicians. We need to ensure that practices across the country are able to continue to operate and provide frontline care that improves health equity and patient access in their communities.”[5] [American College of Physicians]
It is important to note that, as part of the COVID-19 public health emergency (“PHE”), CMS reviewed and identified additional telehealth services to be included on the Medicare telehealth services list. Many of these services, which were set to expire at the end of the calendar year in which the PHE ends, have been extended and expanded in the CY 2022 Final Rule. These changes were praised by commentators as affording practitioners the ability to provide very necessary services to patients while also protecting the health and safety of healthcare providers.
Throughout CY 2021, VMG has observed approximately 50-75% of healthcare organizations delaying in some manner the use of the 2021 WRVU factors in production-based physician compensation models. As healthcare organizations plan their transition to the new WRVU factors, VMG would emphasize an adjustment to the compensation plan that is consistent with the organization’s budget and projected changes to the organization’s reimbursement. It is particularly important to consider the potential long-term impacts on reimbursement as compensation models tend to be fixed for more than one year. Additionally, given the impact of the COVID-19 pandemic on provider compensation and productivity levels, healthcare organizations need to consider the implications of utilizing compensation surveys compiled in 2021, 2022, and potentially beyond. The actual rates per WRVU an organization uses should account for a) the increased WRVU values in the 2022 physician fee schedule, b) the organization’s projected changes in revenue in their 2022 payor contracts and c) market movement in compensation and compensation per WRVU rates.
If an organization uses the 2022 fee schedule without considering any adjustments to the rates it pays employed physicians, the organization risks over-compensating its physicians relative to market. Various factors will impact whether physicians are compensated above levels that might be considered fair market value, so organizations must fully assess the impact of doing nothing and the effect such a move might have on the fair market value and commercial reasonableness of resulting compensation.
Another area of provider compensation that will certainly be impacted by the reimbursement changes is in hospital-based coverage agreements. In many of these agreements, provider groups are already subsidized by hospitals and will likely be requesting additional financial support under the new fee schedule.
The two primary compensation methodologies for hospital-based coverage agreements are collections or revenue guarantees and fixed subsidy models. Under the collections guarantee structure, the contracted provider would bill and collect for professional services rendered and provide periodical reports to the hospital documenting actual professional revenues for reconciliation purposes. Based on the reconciliation methodology and depending on the hospital’s payor mix and service provider’s payor contracts, the changes to the 2022 physician fee schedule could result in significantly lower professional collections for the service provider and, therefore, a larger financial obligation for the hospital.
Alternatively, a fixed subsidy sets the contractual payment in advance by calculating the difference between estimated professional collections and estimated operating expenses. Under this arrangement structure, the provider group bears more risk than under a collections guarantee model because it receives a fixed amount, and hence has to assert more control over containing costs. Under the 2022 physician fee schedule, provider groups that do not receive an adjustment to their existing subsidy contracts could become insolvent if their physicians are unwilling to accept lower compensation for their services.
[1] https://www.amga.org/about-amga/amga-newsroom/press-releases/110321/
[2] Final Rule, Federal Register, November 2021, available at: https://www.federalregister.gov/public-inspection/2021-23972/medicare-program-cy-2022-payment-policies-under-the-physician-fee-schedule-and-other-changes-to-part
[3] https://www.amga.org/about-amga/amga-newsroom/press-releases/110321/
[4] https://www.facs.org/media/press-releases/2021/medicare-cuts-110221
[5] https://www.acponline.org/acp-newsroom/internists-say-2022-medicare-fee-schedule-includes-positive-changes-for-physicians
Subscribe
to our blog