
GenesisCare Bankruptcy Emergence
Christa Shephard
June 11, 2024
Effective October 8, 2024, Carnahan Group has joined VMG Health. Learn more.
August 13, 2024
Written by Savanna Ganyard, CFA; Joshua Miner; Chance Sherer, CVA; and William Teague, CFA, CVA
Cano Health, Inc., headquartered in Florida, is a value-based care delivery platform that specializes in primary care for seniors. In February 2024, Cano announced it would enter a reorganization process under Chapter 11 bankruptcy. Less than six months later, on June 28, 2024, the company announced a successful conclusion of its court-supervised restructuring. The company, now private, is looking forward to a brighter future under a more focused strategy.
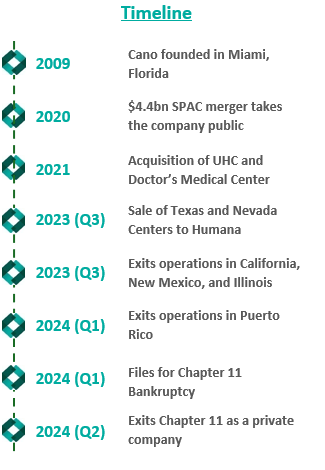
Founded in 2009, Cano began developing its core business as a value-based provider in Florida. The company employs a capitated care model and places a large focus on preventative care and accessibility. The company’s membership is largely comprised of Medicare Advantage, Medicaid, and ACO REACH. As Cano grew, it added complementary service offerings, such as a care management program, a prescription program, and in-home medical visits. These services were meant to prevent hospital admissions and readmissions, increasing Cano’s revenue while decreasing patient total cost of care in the capitated care model.
To further drive growth, the company began to pursue an aggressive policy of expansion through de novo development, acquisitions, and affiliations. The company grew from two markets and 13,700 members in 2017 to 15 markets and 106,000 members by 2020.
In 2021, the company went public in a $4.4 billion merger with a special purpose acquisition company (SPAC) that provided $1 billion in cash proceeds to the company. After going public, Cano continued to fuel growth through acquisitions. In 2021, the company acquired Miami-based University Health Care in a $600 million deal and Doctors Medical Center in a $300 million deal. The company added five states and 121,000 members in 2021, resulting in a total of nine states and 227,000 members. The company continued this growth throughout 2022, ending the year in 10 states and with 310,000 members.
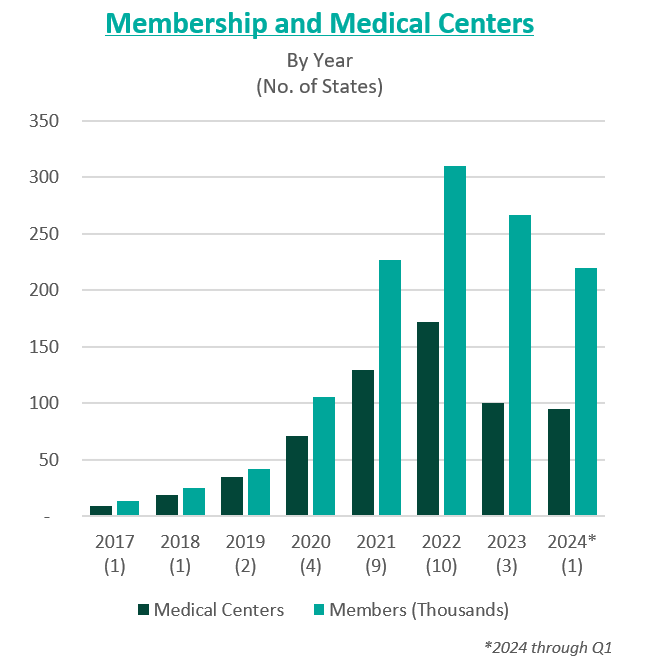
However, in these years of high growth following going public, the anticipated benefits of these acquisitions did not materialize. The company was also affected by industry and regulatory headwinds, including increasing third-party medical costs and a looming Medicare Risk Adjustment Model (V28). On top of these issues, Cano continued to add debt and fell behind on debt repayments. Throughout 2022 and 2023, Cano reported significant losses and an accumulation of $1.2 billion in debt. For context, the company had $1 billion in assets as of December 31, 2023.
In February 2023, Cano entered into a side-car credit agreement with certain lenders. At the end of March 2023, the company’s market capitalization had decreased 90% from its price at the time of its SPAC merger. In April 2023, three board members resigned in protest of company decisions and performance. A couple of months later, the CEO, Marlow Hernandez, stepped down after pressure from shareholders and the former board.
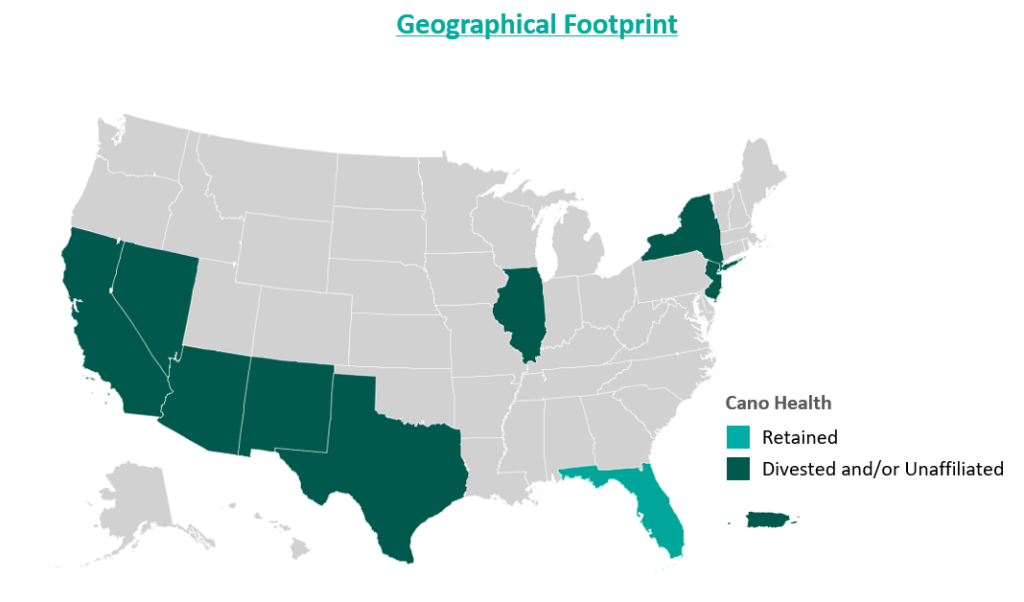
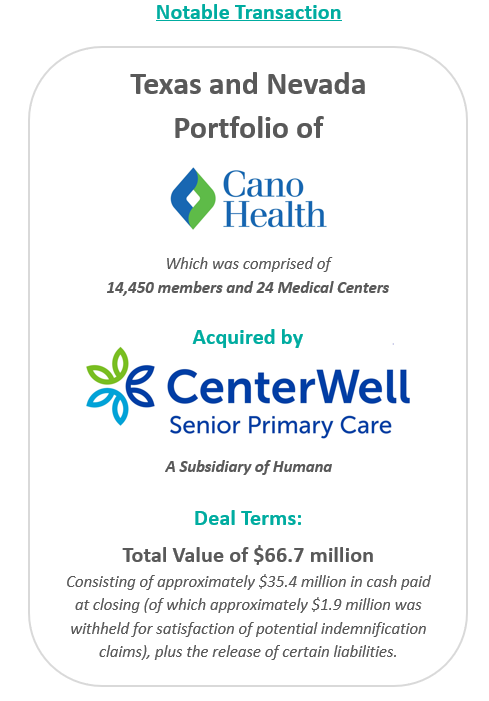
In an attempt improve the company’s performance and cover its liabilities, Cano began to divest its assets. The divestment process began in 2023 prior to the Chapter 11 filing, when the company sold its entire Texas and Nevada portfolio to CenterWell Senior Primary Care, a Humana subsidiary. The net proceeds of the transaction were utilized to pay down debt.
During the second half of 2023, the company also closed medical centers and exited operations in California, New Mexico, and Illinois. These three states represented approximately 5,000 members and 17 medical centers. The company received $19.9 million for the divestiture of certain specialty practices in Florida and assets located in California and Illinois, the net proceeds of which were used as working capital. Cano closed the remaining medical centers in these three states. Finally, Cano successfully exited operations in Puerto Rico at the beginning of 2024.
Despite these transformation efforts, Cano entered into voluntary Chapter 11 proceedings and a Restructuring Support Agreement with most of its lenders in February 2024. The agreement’s primary goal was to reduce debt and position the company for long-term success through cost-cutting measures.
In July 2024, Cano emerged from Chapter 11 as a reorganized private company. The company successfully reduced its debt burden by $1 billion by converting it into equity in the form of common stock and warrants. Additionally, existing investors have contributed an additional $200 million investment to support business operations.
Furthermore, Cano exited its underperforming markets, choosing to focus on its core Florida market. During the bankruptcy process, the court allowed Cano to reject 72 leases in six states. These were sites of offices and medical centers that the company no longer uses.
As established during proceedings, the company’s operational strategy going forward centers around optimizing cost and continuing to evaluate asset performance. To date, Cano is on track to achieve $290 million in cost reductions by the end of 2024. Key drivers of this cost reduction include negotiating with payers, reducing operating costs through decreasing the number of permanent staff, and cutting non-essential spending. In addition, the company is prioritizing Medicare Advantage and ACO Reach lines of business.
Essential to understanding Cano’s emergence from bankruptcy is the amount of divestment the company has undergone. At its peak, Cano operated in nine states and Puerto Rico either directly or through affiliates. To improve operations, the company terminated most of its affiliate partnerships and began to divest many of its operations. Following the reorganization process, the company only operates in Florida. Prior to bankruptcy, Cano had 143 locations in Florida, now reduced to 83 locations.
Cano’s largest asset sale was its centers in Texas and Nevada to CenterWell in a deal worth $66.7 million. At closing, the centers covered 14,450 members and 24 medical centers. These figures imply a multiple of $4,600 per member.
In December 2023, the company commenced a sale process for its ACO Reach line of business. The company has engaged with several bidders, but the transaction has not yet materialized. Cano’s ACO Reach business, which comprises 93,300 members, is projected to achieve $32 million in underwriting margin and $11 million in adjusted EBITDA from August to December 2024. The company also continues to explore sale opportunities related to its Medicaid line of business, which is expected to represent 36,200 members in 2024.
Cano’s financial projections estimate $2.9 billion in revenue and 233,000 members during fiscal year (FY) 2025, growing to $3 billion and 239,000 members by FY 2028. During the same period, the company’s adjusted EBITDA is projected at $125 million, growing to $199 million.
Post-reorganization, the estimated value of Cano at the enterprise level was between $580 million and $720 million. The valuation reflects implied Year 1 (2025) multiples at the midpoint of 5.2x adjusted EBITDA and approximately $2,800 per member.
In June 2024, Cano successfully emerged from bankruptcy as a private company with an improved capital structure and more focused operations. The reduced debt burden, coupled with a $200 million injection of capital, has relieved some pressure on the company as it moves forward. Cano has already made significant progress towards its FY 2024 cost reduction goal, achieving $270 million in cost savings and productivity improvements through the first half of the year. Currently, Cano is focused on its Florida operations but has not ruled out a more prudent expansion in late 2025 or 2026 if it continues to meet its financial goals.
Cano Health, Inc. (n.d.). Press releases, public filings, and investor presentations. Retrieved from www.canohealth.com.
Cano Health. (2023, July 18). Cano Health announces successful emergence from Chapter 11. PR Newswire. https://www.prnewswire.com/news-releases/cano-health-announces-successful-emergence-from-chapter-11-302186063.html
Cano Health. (2023, June 7). Cano Health announces agreement with unsecured creditors committee and court approval of disclosure statement for its reorganization plan. PR Newswire. https://www.prnewswire.com/news-releases/cano-health-announces-agreement-with-unsecured-creditors-committee-and-court-approval-of-disclosure-statement-for-its-reorganization-plan-302152012.html
Cano Health. (2023, March 27). Cano Health enters restructuring support agreement with a significant majority of its lenders to strengthen financial position. PR Newswire. https://www.prnewswire.com/news-releases/cano-health-enters-restructuring-support-agreement-with-a-significant-majority-of-its-lenders-to-strengthen-financial-position-302052889.html
PR Newswire. (2023, March 28). NYSE suspends trading in Cano Health Inc. (CANO) and commences delisting proceedings. https://www.prnewswire.com/news-releases/nyse-suspends-trading-in-cano-health-inc-cano-and-commences-delisting-proceedings-302053778.html
Capital IQ. (n.d.). Investor presentations. Retrieved from Capital IQ website.
Public Information related to Cano Health’s Chapter 11 Plan for Reorganization (Case No. 24–10164). (n.d.). Veritaglobal. Retrieved July 26, 2024, from https://veritaglobal.net/CanoHealth
Klas, M. (2023, July 19). The new Chapter 11 plan for Cano Health aims to exit bankruptcy, cut debt. Miami Herald. https://www.miamiherald.com/news/health-care/article289663459.html
August 7, 2024
Written by Quinn Murray and Ed McGrath, MHA
In the Fall of 2022, we wrote an article discussing not-for-profit health (NFP) system financial performance trends. At the time, NFP systems were experiencing major financial struggles given labor market and supply chain issues coupled with other inflation and industry pressures. While not the primary focus of our 2022 study, VMG Health also raised a concern relative to mid-size hospitals (larger than critical access, but not large enough to provide tertiary/quaternary care). Unfortunately, the concern has proven to be valid as hospital closures and bankruptcies continue. The outlook for these mid-size, independent hospital organizations is not promising given the lack of financial flexibility as larger systems continue the pursuit of acquiring any independent hospitals that have demonstrated any degree of financial success. In 2022, we also noted systems would experience increased competition by private equity–funded niche players and other organizations that could shift profitable services and commercial business from the systems. Their increased presence as disruptors in new markets has accelerated quicker than originally anticipated.
Our 2022 article summarized the financial performance of 21 systems across 32 states, with a combined fiscal year (FY) 2022 operating revenue of $188 billion. As noted in the prior article, the study was not intended to represent a statistically valid sample across all NFP systems, but did include a cross section of systems that provide care to patients in over 30 states with net revenues greater than $2 billion. Of these 21 systems, approximately 15 percent are clients of the VMG Health authors, but the vast majority are not.
Our updated article assesses how those same 21 systems performed in FY 2023 as compared to FY 2022 levels. As a result of this study, our team discovered the importance of understanding the broader implications resulting from the unfavorable financial performance of NFP health systems. This report also discusses the actions our clients and other NFP systems are taking to address the existing financial pressures and to proactively address potential future issues.
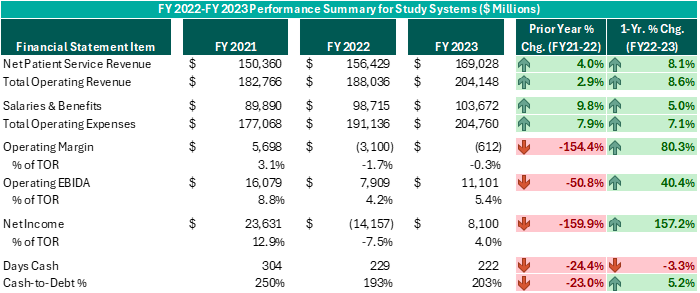
Executive leadership in these systems have made commendable decisions over the past 12–18 months despite ongoing challenges. While operating margins on a combined basis have improved by $2.5 billion from FY 2022 (and combined operating EBIDA improved over $3 billion), these organizations still experienced combined operating losses of ($612 million) in FY 2023. However, while positively trending toward break-even operating margins and 5% or higher operating EBIDA margins is no small feat following the adversity endured nationwide during FY 2022, these levels do not support long-term sustainability. Healthcare systems seeking sustainable financial operations should target operating margins of 3% or higher and operating EBIDA margins of 10% or higher. Those targets may not be achievable for all NFP Health Systems, but consecutive years of operating losses and minimal cash flows are not conducive for strategic growth and reduces an organization’s flexibility to certain strategic investments.
While the performance turnaround noted above is remarkable, the future of NFP healthcare systems continues to be very challenging. Organizations are seeking avenues to develop accretive opportunities to thrive—not just survive. Survival should not be the long-term objective. Systems are exploring and utilizing a variety of options and resources to improve performance, some of which have come to fruition in the past 12–18 months, as evidenced by the financial summary above.
Avenues some of our client system executives have pursued include the following. Note, each market and each situation is unique: One can apply similar approaches, but there is no cookie-cutter or templated solution. Rather, adjust the model to fit the situation as opposed to forcing the situation to fit the model.
To achieve long-term financial success, NFP systems should consider more innovative strategies that complement the evolving healthcare landscape. Patient preferences are not the same as they were 20 years ago, nor is the manner in which healthcare providers deliver care. Competitors and other organizations will capitalize on those who remain complacent and do not adapt. Therefore, sustainable success will require a willingness to adapt to the current industry environment in addition to proactive planning to meet the anticipated future needs of the patients and communities served.
August 6, 2024
Written by Nathan Woods; Frank Fehribach, MAI, MRICS; Kristin Herrmann, MAI, ASA
Healthcare real estate is a critical sector that supports the delivery of medical services, from hospitals and outpatient centers to medical office buildings and nursing facilities. However, this sector is heavily regulated, with specific laws aimed at preventing conflicts of interest and maintaining fair competition. Among the most influential regulations are the Stark Law, antitrust laws, and the federal Anti-Kickback Statute.
The Physician Self-Referral Law, commonly known as the Stark Law, is designed to prevent conflicts of interest in healthcare. It prohibits physicians from referring patients to receive designated health services (DHS) payable by Medicare or Medicaid from entities with which they have a financial relationship, unless an exception applies. DHS includes a wide range of services, such as clinical laboratory services, physical therapy, and radiology. Some exceptions include in-office ancillary services, equipment and office space rental, and bona fide employment relationships. These exceptions must occur within fair market value except certain in-office ancillary services—which simply allow physicians to refer patients for certain ancillary services, such as lab tests or physical therapy—within their own practice.
1. Financial Relationships: The Stark Law targets various financial relationships, including ownership, investment interests, and compensation arrangements. In the context of healthcare real estate, this means that lease agreements, joint ventures, and other financial dealings involving physicians must be carefully structured to avoid prohibited self-referrals. A self-referral in the context of the Stark Law occurs when a physician refers a patient to a medical facility in which they or an immediate family member have a financial interest, such as ownership, investment, or compensation arrangements.
2. Fair Market Value (FMV): All financial arrangements must be at fair market value. Fair market value is the price at which the property would change hands between a willing buyer and a willing seller, neither being under any compulsion to buy or to sell and both having reasonable knowledge of relevant facts. This requirement ensures payments reflect what would be paid in an arm’s-length transaction and are not influenced by the volume or value of referrals.
3. Exceptions and Safe Harbors: Stark Law provides several exceptions that allow for certain financial relationships if specific criteria are met. For example, the rental of office space exception permits arrangements if they are in writing, specify the terms, have a term of at least one year, and meet FMV standards without considering the volume or value of referrals. The bona fide employment relationships exception permits compensation arrangements between physicians and employers if the employment is for identifiable services, the compensation is consistent with fair market value, and not based on the volume or value of referrals. These exceptions are designed to allow necessary and beneficial financial relationships while preventing conflicts of interest.
Stark Law is known for its complexity. Healthcare real estate transactions must undergo careful legal and financial scrutiny to ensure compliance. Violations can result in severe penalties, including fines, exclusion from federal healthcare programs, and the requirement to repay amounts received for services provided in violation of the law.
Case Studies and Precedents
1. Tuomey Healthcare System Case (2015): Tuomey Healthcare System faced one of the largest penalties under Stark Law, amounting to $237 million. The case revolved around improper financial relationships with physicians, where the compensation was linked to the volume of referrals. This case underscores the importance of structuring compensation arrangements to comply strictly with FMV standards and avoiding any link to referral volumes.
2. Scripps Health Case (2021): Scripps Health in San Diego, California settled allegations related to violations of Stark Law. The health system was accused of compensating physicians at rates above fair market value, which were allegedly tied to the volume and value of patient referrals. The settlement amounted to $1.5 million and highlighted the importance of ensuring physician compensation arrangements strictly adhere to fair market value standards and are not linked to referral volumes.
Antitrust laws, including the Sherman Act and the Clayton Act, aim to promote competition and prevent monopolistic practices. These laws are essential in healthcare real estate, ensuring market power is not concentrated in a way that restricts competition or harms consumers.
The Sherman Antitrust Act, enacted in 1890, is the cornerstone of antitrust legislation in the United States. It prohibits certain business activities that federal government regulators deem to be anti-competitive and that restrict interstate commerce and trade. The act broadly prohibits agreements and practices that restrain trade, such as price-fixing, bid-rigging, and market allocation agreements. It also addresses monopolization and monopolization attempts, aiming to promote fair competition, protect consumers from monopolistic practices, and foster economic efficiency.
The Clayton Antitrust Act, passed in 1914, is an amendment to the Sherman Act and further strengthens antitrust laws in the U.S. It focuses on specific practices that the Sherman Act did not clearly address, such as price discrimination and exclusive dealing contracts that may substantially lessen competition. The Clayton Act also prohibits mergers and acquisitions that may substantially lessen competition or tend to create a monopoly. It aims to prevent anti-competitive practices and promote fair competition by addressing various forms of conduct that could harm consumers or competitors in the marketplace.
Implications for Healthcare
1. Market Power and Competition: Healthcare providers acquiring substantial real estate operations must ensure these acquisitions do not unfairly limit competition. For instance, controlling a significant number of facilities in a region could raise anti-trust concerns if it reduces consumer choice or leads to higher prices.
2. Collaborations and Joint Ventures: Partnerships and joint ventures in healthcare real operations can also attract antitrust scrutiny. Such arrangements must be structured to avoid anti-competitive effects, such as price-fixing or market division.
3. Mergers and Acquisitions: Mergers and acquisitions involving healthcare operations are subject to antitrust review. This process involves analyzing market share, potential benefits, and any anti-competitive impacts. Transactions that significantly lessen competition or create monopolies can be challenged and blocked.
Navigating antitrust laws requires a thorough understanding of market dynamics and regulatory requirements. Transactions in the healthcare sector often undergo detailed scrutiny by regulatory bodies like the Federal Trade Commission (FTC). Legal and financial experts must conduct comprehensive market analyses to demonstrate that transactions will not harm competition.
Case Studies and Precedents
1. FTC v. Advocate Health Care Network (2017): The FTC challenged the merger of Advocate Health Care Network and NorthShore University Health System, arguing that it would reduce competition and lead to higher prices for consumers in the Chicago area. The court sided with the FTC, emphasizing the importance of ensuring mergers do not negatively impact market competition.
2. St. Luke’s Health System and Saltzer Medical Group Case (2015): St. Luke’s Health System acquired Saltzer Medical Group, which the FTC argued would reduce competition for adult primary care physician services in Nampa, Idaho. The court ruled against the merger, and St. Luke’s was required to divest Saltzer. This case illustrates the need for careful antitrust review in healthcare mergers and acquisitions.
3. Pennsylvania v. UPMC and Highmark (2014): The state of Pennsylvania filed a lawsuit against UPMC and Highmark, alleging that the two healthcare giants engaged in anti-competitive practices. The case was settled with both parties agreeing to terms that ensured competition in the market, highlighting state authorities’ role in enforcing antitrust laws to protect consumers.
The Anti-Kickback Statute (AKS) is a federal law that prohibits the exchange or offer to exchange of anything of value to induce or reward the referral of business in a federal health care program. This law aims to prevent financial incentives that could corrupt medical decision-making and lead to increased costs for federal healthcare programs.
1. Prohibited Practices: The AKS prohibits any remuneration, including kickbacks, bribes, or rebates, that is intended to induce referrals for services covered by federal healthcare programs. This includes both direct and indirect payments.
2. Safe Harbors: The law provides for certain “safe harbors” that protect specific payment and business practices from prosecution if they meet certain requirements. These include space and equipment rentals, personal services and management contracts, and payments to bona fide employees.
Implications for Healthcare Real Estate
1. Lease Agreements: Lease agreements between healthcare providers and landlords must be carefully structured to ensure they do not involve payments for referrals. For example, rental rates must reflect fair market value and must not be influenced by the volume or value of referrals.
2. Joint Ventures: Joint ventures between healthcare entities and real estate investors must avoid arrangements where returns on investment are linked to the volume of referrals to federally funded healthcare programs.
3. Real Estate Transactions: Real estate transactions must be structured to avoid any implication that payments or benefits are provided in exchange for referrals. This requires detailed scrutiny of the terms and conditions of the transaction.
Ensuring compliance with the AKS requires thorough documentation and a clear separation of any payments from referral activities. Violations of the AKS can lead to severe penalties, including criminal charges, fines, and exclusion from federal healthcare programs.
Case Studies and Precedents
1. United States v. Tenet Healthcare Corporation (2016): Tenet Healthcare settled for $514 million, $368 million for civil penalties, and $145.8 million in criminal penalties to resolve allegations that it paid kickbacks for patient referrals through leasing arrangements. This case underscores the necessity for healthcare real estate transactions to comply with AKS requirements to avoid substantial financial and legal repercussions.8
2. United States v. South Florida Hospital and Healthcare Association (2015): This case involved allegations that a hospital system provided financial incentives to physicians for referrals, which were disguised as above-market rental payments for office space. The settlement highlighted the importance of ensuring that rental payments reflect fair market value and are not tied to referral volumes.
Conducting thorough due diligence and maintaining transparency in financial transactions are essential steps in mitigating risks associated with Stark Law, antitrust laws, and Anti-Kickback Statute compliance. Healthcare business professionals should:
Following established guidelines and best practices can further mitigate compliance risks. Healthcare entities should:
Stark Law, antitrust laws, and the Anti-Kickback Statute play crucial roles in regulating healthcare real estate, ensuring ethical financial relationships and promoting fair competition. While these laws present significant compliance challenges, understanding their provisions and implications is vital for healthcare real estate professionals. By adhering to best practices, conducting thorough due diligence, and seeking expert guidance, stakeholders can navigate these complex legal landscapes effectively, supporting the healthcare real estate sector’s growth and integrity. The case studies and precedents highlight the importance of compliance and the potential consequences of violations, underscoring the need for careful attention to regulatory requirements in healthcare real estate transactions.
HHS Office of Inspector General. (n.d.). Physician self-referral law [42 U.S.C. § 1395nn]. U.S. Department of Health and Human Services. Retrieved from https://oig.hhs.gov/compliance/physician-education/fraud-abuse-laws/
Social Security Act, 42 U.S.C. § 1395 (b) (2024). Retrieved from https://uscode.house.gov/view.xhtml?req=(title:42%20section:1395%20edition:prelim)
Treasury Regulation § 1.170A-1(c)(2), 26 C.F.R. (2024). https://www.law.cornell.edu/cfr/text/26/1.170A-1
Federal Trade Commission. (2017, March 22). Advocate Health Care Network. Retrieved from https://www.ftc.gov/legal-library/browse/cases-proceedings/1410231-advocate-health-care-network
Federal Trade Commission. (2015, February 10). St. Luke’s Health System, LTD, and Saltzer Medical Group, P.A. Retrieved from https://www.ftc.gov/legal-library/browse/cases-proceedings/121-0069-st-lukes-health-system-ltd-saltzer-medical-group-pa
Commonwealth v. UPMC. (2015, November 11). Casetext. https://casetext.com/case/commonwealth-v-upmc
HHS Office of Inspector General. (n.d.). Anti-Kickback Statute [42 U.S.C. § 1320a-7b(b)]. U.S. Department of Health and Human Services. Retrieved from https://oig.hhs.gov/compliance/physician-education/fraud-abuse-laws/
U.S. Department of Justice. (2016, October 3). Hospital chain will pay over $513 million for defrauding United States and making illegal payments. Retrieved from https://www.justice.gov/opa/pr/hospital-chain-will-pay-over-513-million-defrauding-united-states-and-making-illegal-payments
August 1, 2024
Written by Sydney Richards, CVA; Erica Veri
The value a brand brings to a strategic partnership is overlooked in many healthcare joint ventures and affiliations. However, healthcare brands may have a significant impact on a partnership’s success. Healthcare brands can suggest top outcomes to communities in the face of intense competition, attract and retain leading providers, and evoke a sense of loyalty and trust among the patient base. In many joint ventures and partnerships, completing a brand valuation allows the licensor to receive a financial return for their contribution of this important asset. Below, we outlined important factors that may be considered in a brand valuation.
Healthcare brands are commonly contributed to a partnership through a license agreement. The structure and terms of the brand licensure can significantly influence the value. For example, a brand license agreement may stipulate payment terms, which can be structured as an upfront equity in a partnership, a fixed annual payment, or a variable (royalty rate) payment. These terms can have a significant impact on how financial risk is or is not shared between the parties, especially for partnerships such as de novo joint ventures. The license agreement can also specify the duration of the brand contribution and specify whether the rights to the brand are exclusive to the proposed licensee or whether the licensor may enter other brand contributions simultaneously.
From the licensor’s perspective, extending the use of their brand to a partner can offer an opportunity to access a larger patient population without sizable investment in capital and infrastructure. A licensor also gains the opportunity to monetize the positive reputation associated with its brand, which has often been built over significant time, investment in expertise and care quality, and marketing spend. While these historical costs may be difficult to quantify, the quality and strength of the brand, especially as compared to peers, can and should be considered in a brand valuation.
One of the ways the brand strength, recognition, and positioning can be considered in the appraisal is through a “with and without” analysis, which seeks to quantify how forecasted earnings would differ for an opportunity with vs. without using the brand. These earnings can be impacted by items such as speed to ramp up for partnered de novo ventures, increased occupancy or utilization due to the community’s association of the brand with high quality care, margin effects of greater economies of scale, or even a favorable payer mix shift.
Additionally, other benefits may be captured in the with and without analysis, including access to clinical integration, clinical trials and research, facilities and equipment planning, and recruiting. If the licensee is a smaller entity with less market share than the licensor, it may desire to leverage the branding entity’s experience and knowledge of best practices while conveying the expertise and reliability of the larger brand to the patient population.
The cost to replicate considers what it may cost to develop and maintain a comparable brand. While many retail brands communicate price and prestige, healthcare brands typically emphasize a company’s quality patient service, positive outcomes, and reliability. A healthcare brand can also attract physicians and help in retaining talent. These qualities may take years, even decades, to develop. While there are certain quantifiable measures that can be included in a brand appraisal, such as advertising and marketing spend to build and maintain a brand, it can be difficult to measure the true costs to replicate brand value for many healthcare brands. Additionally, unless the licensee can generate a return on these costs, it would not be reasonable to assume they would be willing to pay for all historical costs unrelated to a particular licensing arrangement. As a result, this approach is commonly considered but may not directly drive a value indication for the specific payment a licensee should make for the use of the brand.
A licensee’s financial performance may have a material impact on the amount it can expect to pay in a licensing arrangement. Factors such as business stage (start up, growth, or mature), subindustry, margin, and operational capacity or constraints can directly impact the ability of a brand to drive incremental earnings to the licensee through use of the brand. A brand valuation for a license payment between two entities commonly includes a thorough examination of the licensee’s position in the local and greater market, performance compared to peers, and outlook.
There are numerous market sources for brand valuation comparables. While commonly considered and thoroughly analyzed, due to the uniqueness of each licensing opportunity, many lack direct comparability to the royalty rates published in publicly available databases, such as MARKABLES, ktMINE, and Scope Research. To the extent that there are brand comparables, a brand valuation should consider reasonable market ranges for similar assets and transactions.
Compared to many healthcare business or other asset valuations, healthcare brand valuations can be difficult. There can be uncertainty (and differences of opinion) on the go-forward impact a brand may have on a business. Although there are established general market ranges within healthcare segments, there are less direct market comparables compared to other partnership contributions, such as business equity or real estate value, for brands. With VMG Health on your team, you can expect the quality, responsiveness, and expertise your brand deserves to overcome these hurdles and drive a successful brand contribution and lasting partnership.
July 31, 2024
Written by Jordan Nelson
The following article was published by Retina Today.
In recent years, the field of ophthalmology, including the subspecialty of retina care, has witnessed significant transformations driven by private equity (PE) investments. This trend has led to a multitude of changes, both positive and challenging, in how retina practices are structured, managed, and perceived. As these investments continue to shape the landscape, it becomes crucial to examine their effect on patient care. Doing so will help health care providers navigate these practice management changes to ensure that patients continue to receive the highest quality care.
PE firms have become increasingly interested in investing in medical practices, including those specializing in retina care. These PE investments are typically structured through the creation of a Management Services Organization (MSO) that acquires the assets of medical practices while keeping practice entities in place for regulatory purposes.
MSOs provide a range of services to medical practices, such as human resources (HR), revenue cycle management, finance, and accounting. The MSO also provides capital for expansion, while implementing operational changes to improve profitability. Typically, physician owners who sell their practice assets to an MSO reinvest a portion of their sale proceeds into the MSO entity, thus becoming co-investors and part owners alongside the PE firm.
By far, the largest retina MSO is Retina Consultants of America (RCA). RCA received PE funding from Webster Equity Partners in 2020. Today, RCA holds 23 acquired brands, 200 locations across the United States, and hundreds of retina specialists.1 Prism Vision Group, another PE-backed MSO, was initially known as New Jersey Retina prior to being funded by Quad-C Management in 2018. This MSO has made 21 acquisitions, primarily retina practices, but also general ophthalmology practices and ambulatory surgery centers in the Northeastern United States.
Nearly 40 PE-backed eye care MSOs operate in the United States, and nearly all partner with and employ retina specialists, many of whom are part of general ophthalmology groups. Hundreds of millions have been invested in these platforms, which has created a significant shift in how retina practices are managed and operate, with implications for both physicians and patients.
At a Glance
While PE investments can bring financial benefits and operational efficiencies, they also pose several challenges for medical practices. PE ownership often has an investment horizon of 5 to 7 years to produce a +25% return for investors. New management is often hired, bringing with it business management tools that smaller practices may not be used to using, such as annual budgets and board approval for strategic initiatives. PE also requires uniform information systems, leading to significant changes to accounting, practice management, and health record systems.
The C-suite executives of an MSO are incentivized by profitability and enterprise growth. If not careful, an MSO may begin to prioritize process, systems, and profitability over patient experience and outcomes. Administrative burdens and standardized protocols may not align with the personalized approach often associated with medical specialties such as retina care. Downward financial and administrative pressure on physicians can also lead to a lack of clinical excellence.
Despite these challenges, there are strategies physicians and practices can employ to ensure that patients continue to receive excellent care under corporate ownership.
It is not feasible for every physician in a practice that employs dozens (or even hundreds) to have clinical control over the organization; as an alternative, MSOs can establish a Medical Executive Committee (MEC). This is a committee comprised strictly of physicians and has direct access to the MSO’s Board of Directors.
The committee is tasked with representing the general mind of the physicians and ensuring clinical considerations remain a top priority. The MEC works with management to establish annual budgets for new equipment or other technology investments. The MEC is charged with establishing clinical best practices and protocols, monitoring quality metrics, and addressing HR situations that affect clinical care. The goal is to ensure physicians have independent representation at the highest levels of the organization and the clinical autonomy of providers remains sacrosanct.
In some MSOs, the Board of Directors has physician representation, which is good, but not a substitute for an MEC. Within general ophthalmology practices, specialties like retina should be appropriately represented. Geographic representation should also be given consideration, and as MSOs grow, geographic sub-MECs could be useful.
Physicians’ interaction with each other can create a culture of collaboration and accountability. Collaboration often leads to innovative solutions to the challenges physicians face as part of a PE partnership model. Establishing a regular cadence for collaboration can facilitate the open exchange of ideas among care providers. Monthly or quarterly conferences/video calls allows providers to share ideas around clinical quality, new technology or techniques, hiring and staffing best practices, and a general forum to discuss treatment plans for uncommon or difficult patient situations.
In-person collaboration and meetings can also be a positive addition to the practice. While far more expensive than a conference call, face-to-face meetings offer a more personal and concentrated format for physicians to engage with each other.
Corporate-owned practices should support physicians’ continuing education to ensure they stay abreast of the latest advancements in retina care. This can help maintain high standards of care and physician clinical autonomy. At a minimum, practices should include a budget for providers to attend conferences and other education events.
In addition, company management can coordinate with the MEC to create internal education opportunities and training. This might include inviting internal experts to share their knowledge with the broader group or inviting outside industry participants such as academia, health systems, or technology companies to collaborate.
The initial success of most independent practices is dedication to creating a great patient experience. This standard, regardless of ownership, should always be the primary focus. Not only is this the right thing to do for patients, but also for the business.
Building and maintaining a patient-first culture is done by setting the example at the top of the organization. Board of Director and shareholder meetings should allocate as much time to patient-related matters as they do to financial and strategic items. For example, in a one-hour Board of Directors meeting, it is not unreasonable to expect 20 minutes of the agenda to focus on items such as quality metrics, patient satisfaction surveys, and clinical innovation. Much of this can be addressed by the MEC in board meetings.
Corporate-owned practices should establish quality metrics that prioritize patient outcomes and satisfaction. This will likely require investment in staff and technology to collect and analyze data. If knowledge is power, data can be the key to understanding how a practice is succeeding or failing and where it is happening across the platform. Regular monitoring and assessment of these metrics can help identify areas for improvement and ensure high-quality care.
Open and transparent communication between physicians and their local practice administrators is crucial. Just as physicians need dedicated access to the Board of Directors, local practice operators need direct access to the physicians in the practices they are charged with operating. Local practice administrators are on the front line when identifying problems and effectively rolling out new programs. Without effective and open communication, much can get lost between the siloed roles in which administrators often operate.
In the Literature
A recent study published in Ophthalmology found that, after retina practices are acquired by PE, their Medicare spending increases. The researchers looked at a total of 82 practices acquired by PE during the study period (2015-2019) and matched control practices. In the PE-acquired practices, they found a 22% increase, per practice-quarter, in the use of higher-priced anti-VEGF agents (i.e., aflibercept [Eylea, Regeneron]), compared with control, non-PE, practices. This increased usage, averaging an extra 6.5 injections, led to an increase in overall Medicare spending of $13,028 per practice quarter, or 21%.
Practices should empower patients to advocate for their own care. This includes educating patients about their condition, treatment options, and how to navigate the health care system to ensure they receive the best possible care. Patients should have the ability to provide feedback about their experience. Technology can play an important role in patient advocacy, but dedicated staff tasked with patient advocacy is often the best approach to ensure patients have what they need to feel their experience is the priority of the practice.
PE investment in retina practices is here to stay, and it represents a significant shift in the health care landscape. While these investments bring opportunities for growth and efficiency, they also pose challenges for patient care. By prioritizing patient welfare, preserving physician autonomy, and maintaining high standards of care, practices can navigate these changes and ensure that patients continue to receive great care under corporate ownership.
BSM Consulting. Internal Report. 2024.
Prism Vision Group. Accessed April 22, 2024. prismvisiongroup.com
Retina Consultants of America. Accessed April 22, 2024. www.retinaconsultantsofamerica.com
Singh Y, Aderman CM, Song Z, Polsky D, Zhu JM. Increases in Medicare spending and use after private equity acquisition of retina practices. Ophthalmology. 2024;131(2):150-158.
July 23, 2024
Written by Matthew Marconcini, CPA
Selling your company can be an exciting time, filled with potential opportunities for growth and new horizons. Whether your company is accrual based, following GAAP, or it reports on a cash basis, proper preparation for the sale of your company is extremely important. This journey often involves a complex web of financial transactions and negotiations, with numerous parties at the table. Among the critical elements in this process are financial due diligence and performing a quality of earnings (QOE) analysis. The QOE process is a critical aspect of financial reporting and analysis that helps stakeholders, like investors and creditors, assess the reliability and sustainability of a company’s reported earnings.
The QOE analysis can play a pivotal role in shaping the outcome of the sale and can significantly impact the perceived value of your business. Therefore, as management, it is essential to be well-prepared and proactive in assessing and evaluating the quality of your business’ earnings, as it influences the selling price and builds trust and confidence among potential investors and other stakeholders. We have outlined eight steps management can take to best prepare for the QOE process.
Management should have a clear understanding of what QOE means. It assesses the underlying economic substance of reported earnings, ensuring they are not distorted by accounting manipulations or one-time events.
Accurate financial record-keeping is fundamental to high-quality earnings. Management must ensure that financial statements are free from material misstatements and that all transactions are properly recorded.
Transparency is crucial. Ensure all material transactions, both positive and negative, are adequately disclosed in the financial statements and related footnotes.
Maintain consistency in financial reporting practices. Frequent changes in accounting policies can raise questions about the QOE. If policies do change, explain the rationale behind it and the financial impact of the change.
Recognize revenue in accordance with accounting standards only when it’s earned and realizable. Avoid prematurely recognizing revenue or engaging in overly aggressive practices. If your company reports on a cash basis, pulling together the proper data that will show revenue based on date of service rather than the collection date will be key.
Clearly distinguish between one-time or non-recurring events and ongoing operations in financial reporting. Disclose the nature and impact of such events to prevent misinterpretation.
Be prepared to provide a comprehensive and honest analysis of the company’s financial results. Explain the drivers of earnings, changes in accounting policies, and potential future risks and uncertainties. The more support you can provide related to both historical performance and future growth initiatives, the more accurate and comprehensive your analysis.
Take the time to review the various systems used to operate the business and start pulling data together. If certain systems are maintained by third parties, informing them of the situation and discussing what they need to do will create a smoother process. If certain reports don’t have the necessary inputs or data, be prepared to discuss that and what alternative information would be useful.
By considering these guidelines and implementing the underlying thought processes, management can best prepare for the QOE process, demonstrating a commitment to transparency, accuracy, and integrity in financial reporting. This, in turn, builds trust and credibility with investors and other stakeholders, creating a smooth transaction process for management.
June 13, 2024
Written by Johnny Zizzi, CPA; Lukas Recio, CPA
When considering a new acquisition or transaction, accurate financial reporting is paramount for informed decision making. One significant aspect of financial reporting is the choice of accounting method: cash, accrual, or a hybrid of both. Many companies begin their journey with cash accounting, but as they grow and evolve or are otherwise acquired by a larger entity, they often transition to accrual accounting to meet regulatory requirements or achieve a more comprehensive financial picture.
This transition is not without its pitfalls and considerations, particularly when understanding its impact on enterprise valuation resulting from the quality of earnings process. Key considerations when converting from cash to accrual accounting include revenue recognition in accordance with ASC 606, expense accrual recognitions, managing changes in working capital, and earnings volatility.
Cash accounting, also called checkbook accounting, entails recording transactions when cash changes hands, which provides management with a straightforward method for tracking cash flow. Small businesses often prefer this method because the IRS allows it when certain size criteria are met and because it is easier to track money as it moves in and out of bank accounts. Further, there is no need to evaluate accounts receivable or payable to determine income when using cash accounting, simplifying the management of the financial statements as a whole.
However, for healthcare entities, this simplicity can be misleading, as it does not capture the true financial obligations and revenues tied to patient care and insurance reimbursements. Accrual accounting, on the other hand, records revenues when they are earned and expenses when they are incurred, regardless of when cash is exchanged. While cash accounting may be simpler for small businesses, accrual accounting offers a more accurate representation of a company’s financial health, especially as they grow and become more complex.
A crucial component of most healthcare services transactions is the quality of earnings analysis, which aims to assess the sustainability and accuracy of historical earnings and the achievability of future earnings, thereby providing potential buyers with a clear understanding of the company’s true earning potential.
Transitioning from cash-basis accounting to accrual accounting entails significant differences and challenges in revenue recognition. Under cash-basis accounting, revenue is recognized when cash is received, while accrual accounting dictates recognition when revenue is earned, irrespective of cash-flow timing. This shift necessitates adjustments to accurately reflect revenue generated within a given period, especially for long-term contracts or services rendered where cash receipts may occur at different points from when the revenue is earned. Challenges arise in estimating and timing revenue recognition, requiring careful assessment of performance obligations, delivery, and collectability.
Issues stemming from the diverse revenue streams and payment models prevalent in healthcare, such as fee-for-service, capitation, and bundled payments add an additional layer of complexity when converting from cash to accrual accounting, as each payment model has distinct timing and recognition criteria. Additionally, healthcare entities often engage in complex contractual arrangements with payors and providers, leading to variations in revenue and expense recognition practices. Moreover, healthcare organizations may have unique regulatory requirements and accounting treatments for certain transactions, further complicating conversion efforts.
Differences in case mix, payor mix, and procedure mix among healthcare entities can also impact revenue recognition as the collectability of outstanding accounts receivable is often different for specific payor and case mixes. Cash waterfalls, zero-balance analyses, and other revenue hindsight analyses are leveraged as part of VMG Health’s comprehensive quality of revenue analysis to ensure revenue recognition is converted from a cash basis to an accrual basis in accordance with ASC 606. Adherence to revenue recognition principles, while requiring meticulous analysis to mitigate misinterpretation and manipulation, is a critical component to a quality of earnings analysis, as it ensures financial statements provide a more comprehensive view of revenue performance, enhancing transparency and comparability. For further detail on quality of revenue analysis, see VMG Health’s previous article: Proceed with Caution: Five Key Considerations in Quality of Revenue Analysis.
Transitioning from cash to accrual accounting presents unique challenges beyond revenue recognition. One significant hurdle lies in accurately accounting for expenses, particularly in healthcare facilities where costs often span various departments and service lines. Accrual accounting requires recognizing expenses when incurred, irrespective of cash outflows, which can be intricate in healthcare settings due to the complex nature of patient care, procurement of medical supplies, and maintenance of facilities. Ensuring accountants properly match expenses to the periods in which they contribute to patient care or administrative functions may require complex allocation and estimation methodologies.
For instance, the timing and recognition of expenses related to medical supplies and pharmaceuticals can vary based on inventory management practices and rebate arrangements with suppliers. Historical cost of goods sold analysis and margin analysis are two of the most common strategies implemented to understand underlying changes in the business, providing a basis for accurately matching expenses to the relevant accounting periods. In large healthcare systems, these complexities are further amplified by the need to allocate costs accurately across multiple departments and service lines, such as inpatient, outpatient, surgical, and emergency services. Addressing expense accrual challenges necessitates a comprehensive understanding of healthcare operations and collaboration between finance and operational personnel to ensure the accuracy of accrual conversions.
In the context of a transaction, small businesses may prepay (malpractice insurance) or pay after the fact (common area maintenance charges) for certain expenses, which must be converted to an accrual basis to properly inform a buyer of the business’ financial condition.
Shifting from cash to accrual accounting also affects the management and assessment of working capital. Under cash accounting, working capital appears straightforward, often mirroring the cash flow directly. However, accrual accounting requires a more nuanced view, recognizing accounts receivable, accounts payable, and inventory changes that may not have immediate cash implications but significantly impact liquidity and operational efficiency. Accurate tracking and managing these elements is crucial, as they influence a healthcare organization’s true financial position and operational performance and may have purchase price implications.
Understanding and converting net working capital on an accrual basis also helps shareholders and potential buyers identify a business’ strengths and potential weaknesses. For healthcare entities, a rise in accounts receivable under accrual accounting indicates future cash inflows but also highlights the importance of effective revenue cycle management, including timely billing and collection processes. Similarly, accounts payable under accrual accounting provide insights into a company’s obligations and upcoming cash outflows, lending toward robust vendor management and procurement practices. Healthcare entities must develop comprehensive systems for monitoring these working capital components to ensure they reflect the actual financial health and to make informed decisions regarding cash management, investment opportunities, and strategic planning. However, there must first be benchmark net working capital to compare future trends.
Under cash accounting, earnings may appear more volatile, as revenues and expenses are recorded only when cash transactions occur. However, accrual accounting captures economic events more accurately and consistently. Fluctuations in reported earnings can be caused by timing differences in revenue and expense recognition and can be particularly pronounced in the healthcare sector, where seasonal variations and payor reimbursement lags are common, causing revenue to be recognized in one period and the corresponding expenses in another on a cash basis of accounting.
For stakeholders and potential investors, understanding the sources and implications of this volatility is crucial for assessing the company’s true financial health. Cash-to-accrual conversions within a quality of earnings analysis help identify and normalize these fluctuations, providing a clearer picture of sustainable earnings and operational performance. By aligning revenue and expense recognition to an accrual basis, stakeholders can benefit from more reliable insights into the company’s financial trajectory, aiding better investment and management decisions. For healthcare entities, this detailed analysis is particularly vital, given the sector’s unique financial dynamics and regulatory landscape. The application of advanced analytical techniques, such as trend analysis and scenario modeling, can further enhance the understanding of earnings volatility and its impact on long-term financial planning and stability.
Converting from cash accounting to accrual accounting in a quality of earnings analysis offers several positive benefits. Accrual accounting provides a more accurate reflection of a company’s financial performance by matching revenues and expenses to the periods in which they are earned or incurred, offering a clearer picture of the company’s profitability over time. This enables stakeholders to make better-informed decisions regarding operational changes, investment, lending, or acquisition opportunities. Additionally, accrual accounting enhances comparability with industry peers and facilitates benchmarking analysis, as financial statements prepared under an accrual basis are inherently more standardized and comparable. Moreover, accrual accounting can uncover trends and patterns in revenue and expense behaviors, providing deeper insights into the company’s underlying financial health and operational efficiency. Overall, the conversion to accrual accounting strengthens the transparency, reliability, and credibility of earnings analysis, fostering trust among investors, creditors, and other stakeholders.
June 11, 2024
Written by Timothy Kent, CVA; Jordan Tussy, CVA; Molly Smith
GenesisCare, a prominent provider of cancer services worldwide, filed for voluntary reorganization under Chapter 11 of the U.S. Bankruptcy Code on June 1, 2023, in the United States Bankruptcy Court for the Southern District of Texas (Case No. 23-90614). The Australian-based company, once valued at $5 billion and backed by private equity firm KKR, faced financial difficulties due to high debt levels and operational challenges.

Founded in 2004 by Dan Collins, GenesisCare (the “Company”) served Australian cancer patients until 2015, when the Company expanded to Europe via its purchase of eight cancer centers from Cancer Partners UK. During 2016, GenesisCare continued growing its European operations through the acquisitions of 17 centers in Spain from IMOncology and Oncosur Group.
In late 2019, GenesisCare made headlines with the acquisition of U.S.-based cancer provider 21st Century Oncology for $1.5 billion. Two years prior, 21st Century Oncology filed for bankruptcy because of declining reimbursement and “regulatory costs concerning electronic records and legal expenses.” At the time of acquisition by GenesisCare, 21st Century Oncology operated 294 locations, including 124 radiation oncology centers, with an estimated $230 million of earnings before interest, tax, and depreciation (EBITDA).
While rapidly expanding GenesisCare’s footprint, the 21st Century acquisition left the Company with significant levels of debt and a new operations base that was reemerging from bankruptcy. GenesisCare faced significant challenges in its effort to turnaround the U.S. operations, including an aging equipment base and IT system, operational inefficiencies, and increased competition. Prior to GenesisCare’s Chapter 11 filing, they reported approximately $2 billion of total debt on its balance sheet, largely associated with the 21st Century acquisition.
In March 2023, CEO and Founder Dan Collins stepped down, and three months later, the Company filed for bankruptcy on June 1, 2023.
Five months after its initial filing, GenesisCare announced the U.S. Bankruptcy Court for the Southern District of Texas confirmed the Company’s Chapter 11 Plan of Reorganization after receiving support from approximately 95% of voting creditors. The plan included significant deleveraging of GenesisCare’s balance sheet, with a reduction in total debt by approximately $1.7 billion.
On February 16, 2024, GenesisCare completed its reorganization process and emerged from Chapter 11. As part of its reorganization plan, GenesisCare will operate as four distinct businesses in the U.S., Australia, Spain, and the UK, with an independent governance structure and Board of Directors for each business. Furthermore, the businesses will be responsible for the strategies and performance of their market. The Company also received approximately $56 million of new capital infusion from investor groups to help support the growth of the remaining businesses. As a result of the restructuring plan, the Company is prepared to move forward well capitalized with a relatively low level of debt and a more focused operational strategy.
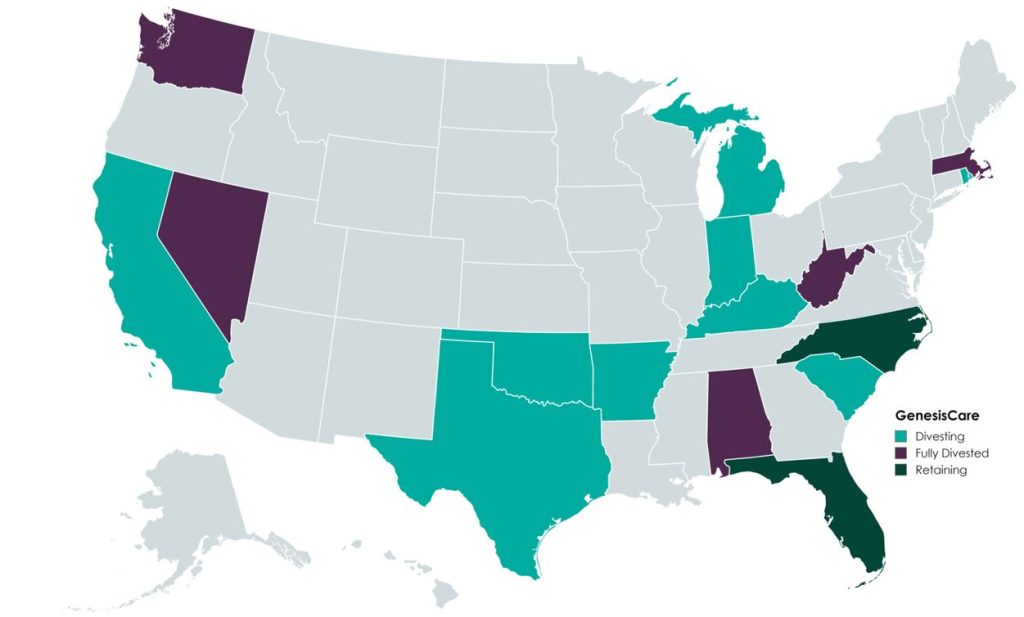
In the U.S., GenesisCare will retain practices in the “fast-growing markets” of Florida and North Carolina, which will continue to offer similar cancer care services (medical oncology, radiation oncology, surgery, and imaging). Currently, the Company operates 145 locations across the two states. GenesisCare has sold or is in the process of divesting its remaining assets across 14 states.
Newly appointed chief executive officer David Young said, “I am confident that our independently run businesses are strongly positioned to capture the exciting opportunities available to them in the markets they serve while never losing sight of our core goal: delivering better life outcomes to patients.”
A primary objective of GenesisCare’s restructuring plan was to divest all U.S.-based assets outside of North Carolina and Florida. This decision was part of its strategic plan to focus on core operations to ensure long-term sustainability.
According to bankruptcy filing documents, GenesisCare has divested 32 locations across 14 states. Assuming all of the transactions close at the defined purchase price in the transaction agreements, cash proceeds to GenesisCare would be approximately $113 million, with an implied equity value of approximately $131 million (see chart below). The assets have drawn interest from many different buyer types, including health systems, large oncology platforms, and practices. Dr. Shaden Marzouk, President of GenesisCare U.S., said, “The strong interest we received from a wide variety of buyers from across the U.S. is a reflection of what we have long known―that GenesisCare’s U.S. business benefits from an incredible team, a desirable footprint and a proven ability to care for patients.”

One notable transaction was OneOncology’s acquisition of two radiation oncology practices in South Carolina for $25.0 million (per the asset purchase agreement), expanding OneOncology’s service offerings in an existing market. CEO of OneOncology, Jeff Patton, MD, said, “For OneOncology, these are two great business assets that are really the only radiation facilities that are open in that market. It’s a market we were already in, so sometimes things match up well.” Specifically, OneOncology acquired a Myrtle Beach facility with three linear accelerators and a Conway Center with one.
California-based Sutter Health purchased five radiation oncology practices in Modesto, San Luis Obispo, Santa Cruz, Stockton, and Templeton, California. According to the purchase agreement, the total purchase price for these centers was $32 million. President and CEO of Sutter Health, Warner Thomas said, “We know how important it is for specialty services like cancer care to be offered close to home so patients can stay on track with their treatments. Keeping continued cancer care accessible in these communities was a driving force for Sutter to acquire these care centers.” Sutter also has certain capital investments in mind, including new radiation oncology equipment, technologies, and other support services.
Based on Kroll’s bankruptcy docket, there are medical and radiation oncology assets still available for sale, which could result in increased transaction activity with interest buyers, such as health systems, private equity–backed oncology platforms, and practice acquisitions. After successfully emerging from Chapter 11, GenesisCare is entering a new chapter, as emphasized by CEO David Young: “GenesisCare has achieved the goals it set out at the beginning of its restructuring process. We exit Chapter 11 with great businesses, each with a compelling future.” The Company’s focus on continuous growth is highlighted by the planned construction of three new radiation oncology centers in Australia, scheduled to open in 2024. With a more concentrated U.S. and global platform, GenesisCare has indicated that it is well positioned for future growth as a newly capitalized, low-debt entity committed to providing the highest level of care for its patients.
Patrick, A. (2024, February 18). GenesisCare emerges from bankruptcy, cuts deal with government. Australian Financial Review. Retrieved from https://www.afr.com/companies/healthcare-and-fitness/genesiscare-emerges-from-bankruptcy-cuts-deal-with-government-20240218-p5f5t5
Staff Writer. (2024). Amid major cancer care bankruptcy, oncology clinics sold. Oncology News Central. Retrieved from https://www.oncologynewscentral.com/article/amid-major-cancer-care-bankruptcy-oncology-clinics-sold
GenesisCare. (2024). GenesisCare’s reorganisation plan confirmed with overwhelming support from voting creditors. GenesisCare. Retrieved from https://www.genesiscare.com/au/news/genesiscare-reorganisation-plan-confirmed-with-overwhelming-support-from-voting-creditors
GenesisCare. (2024). GenesisCare completes reorganisation and emerges from Chapter 11. GenesisCare. Retrieved from https://www.genesiscare.com/au/news/genesiscare-completes-reorganisation-and-emerges-from-chapter-11
Patrick, A. (2019, December 13). Aussie cancer outfit makes first US move in $1.5b deal. Australian Financial Review. Retrieved from https://www.afr.com/companies/healthcare-and-fitness/aussie-cancer-outfit-makes-first-us-move-in-1-5b-deal-20191213-p53js7
Private Equity Stakeholder Project. (2024). Private equity healthcare bankruptcies are on the rise. Private Equity Stakeholder Project. Retrieved from https://pestakeholder.org/reports/private-equity-healthcare-bankruptcies-are-on-the-rise/
June 4, 2024
Written by Frank Fehribach, MAI, MRICS; Danny Cuellar
There was once a time when no one considered a lease as an asset. It was just an expense to be paid at the end of the month and ignored until the following month. Then ASC 842 came around in 2018 and operating leases became assets—right-of-use assets (ROUs), to be exact. ROU assets had to be put on the balance sheet and depreciated. Then they had to be tested for impairment. Now, for some firms that are downsizing their operations (or downsizing their physician practices), they must be impaired.
In the beginning, there was FAS 13, Accounting for Leases. For lessees, leases were either operating or capital leases. Operating leases were expensed and capital leases, if they passed the test, were put on the balance sheet. To be a capital lease, you had to meet one or more of the four criteria:
FAS 13, which came into effect in 1977, became known as ASC 840 under the codification of the accounting standards. ASC 840 would continue until it was replaced by ASC 842 in 2019 for public companies and 2021 for private companies. ASC 842 was developed over nearly a decade and released in 2016. The main difference between the ASC 840 and 842 was that all operating leases greater than 12 months in term would be recognized on the balance sheet as both an ROU asset and a liability. The Financial Accounting Standards Board had hoped this difference would increase transparency. It certainly had the effect of producing large lease guidance manuals from all the major accounting firms. It also produced a whole new category of assets that potentially need to be tested for impairment, and to be impaired if they failed.
Accounting firm guidance indicates that ROU assets are subject to ASC 360-10 impairment guidance applicable to long-lived assets. ROU assets must be assessed for potential impairment if there is an internal or external indicator, like the decision to vacate a leased space entirely or partially. However, vacating a leased space does not mean that it has been abandoned. Abandonment accounting would only apply if the space were vacated and not used at all (even for storage) without intent to sublease the space.
ASC Topic 360, Property, Plant, and Equipment was issued in August 2001. Because of ASC 842, former operating leases of more than one year are now long-lived assets. These leases are subject to the same asset impairment guidance in ASC 360 that applies to any other property, plant, and equipment assets. ASC 360-10-35-23 states, “For purposes of recognition and measurement of an impairment loss, a long-lived asset or assets shall be grouped with other assets and liabilities at the lowest level for which identifiable cash flows are largely independent of the cash flows of other assets and liabilities.”
An ROU asset has identifiable cash flows based on the lease payments. Testing is performed based on an undiscounted cash flow. During normal business operations, leased space is often vacated as operations are right-sized to the current business environment, creating a need to test for impairment. If the undiscounted cash flow is lower than the carrying amount of the asset, ASC 360 requires the owner of that ROU asset to reduce it to its fair value.
What is the fair value of an ROU asset that is no longer used for the purpose that it was created for through the lease? To answer this question, we must know what market participants would pay for this asset if offered on the market as of the trigger date. For an ROU asset, this would be a sublease and the present value of future sublease payments. Typically, there is a certain period to find a sublease tenant, and then the sublease tenant would occupy the space for the remainder of the primary term. Option periods, that before may have been included in the ROU asset, may be excluded because the landlord may not allow it, or the actual tenant may want to end the lease and not exercise an option. If option periods were included in the ROU asset value originally, the impairment amount would increase. Additionally, the discounting of the sublease payments is done at a market rate not an internal borrowing rate (IBR) used to establish the ROU asset value initially.
During a lease term, an organization’s operations in the leased space can be completely shut down or downsized. Typically, a completely vacated space will fail Step 1 of the testing, as there is no cashflow being generated for the lease space. For a partial vacancy, the Step 1 test becomes even more important, as part of the space is still being utilized. However, our experience is that a partially vacated space will still trigger the need to test for impairment. For a completely vacated lease, there is usually the assumption that the ROU asset must be impaired.
In this new world of ROU assets, health systems need to be wary of physician practice downsizing in a leased space. Downsizing in a leased space could and should trigger impairment testing and possibly adjustment to fair value. The transition to ASC 842 represents a significant shift toward greater transparency in lease accounting, as the new standards provide a clearer picture of an entity’s financial obligations, though they also require more complex accounting. VMG Health has extensive experience assisting health systems and physician practices with this financial reporting exercise.
May 29, 2024
Written by Isabella Rosman and Tim Spadaro, CFA, CPA/ABV
The following article was published by Becker’s Hospital Review.
Throughout VMG Health’s client base, we are privileged to work with many major players across the physician practices landscape—from solo practitioners and independent physician groups to large platform practices, private equity (PE)–backed physician practice rollups, and those affiliated with large health systems.
VMG Health has been engaged to assist clients in varying capacities associated with transactions, ranging from providing business valuations to financial due diligence (quality of earnings). This insight has provided important visibility into the buyer’s perspective. Further, our work has delved into the operations of practices, including coding and compliance, physician compensation, and strategy work. As a result, our experience offers us a unique glimpse into physician practices and the underlying transaction environment. From our experience, including anecdotal discussions with clients and operators in this space, we’ve outlined a few major headwinds and tailwinds facing physician practice transactions in 2024.
Reimbursement Pressure: Physician practices continue to face reimbursement pressure. In November 2023, the Centers for Medicare & Medicaid Services (CMS) issued its final rule announcing policy changes for Medicare payments under the Physician Fee Schedule (PFS) for 2024. Per CMS, overall payment rates under the PFS will be reduced by 1.25% in 2024, following a 2.0% decline in 2023. Although the overall impact on reimbursement varies across specialties, the rate cuts will continue to suppress margins and put pressure on physician practices. For more information on operational challenges and opportunities with physician practices, see VMG Health’s most recent Physician Alignment Tips & Trends Report.
Persistent Inflation: Wage inflation (largely driven by a tight labor market, an aging physician base, and recruiting challenges) and the rising costs of drug and medical supplies have been persistent. According to the government’s Medicare Economic Index (MEI), medical practice costs are expected to increase by 4.6% in FY 2024 on top of last year’s 3.8% increase. Without reimbursement keeping pace with increasing costs, many physician practices’ profit margins have contracted.
Many physician practices seek out a partner to help combat the daily pressures they face. Practices may benefit from operational synergies by consolidating with a larger organization, particularly if the larger organization has favorable reimbursement rates or anticipated cost savings from duplicate services (back-office employees, external accounting, etc.). In fact, many buy-side clients run a managed care or “black box” analysis to assess the potential rate lift and the resulting practice economics on a post-transaction basis to better inform themselves and their investment committees during diligence. Contact VMG Health’s Revenue Consulting & Analytics team to analyze the potential rate lift on your next deal.
Record High Dry Powder: PE has been an active participant in the physician practice transaction space for many years, as evidenced by recent deal volume presented in the table below. Capital committed to PE funds but not yet deployed (dry powder) is presently at record highs for healthcare services. The current estimate of dry powder earmarked for healthcare services among U.S. headquartered PE managers is approximately $100 billion, according to Pitchbook’s Q4-2023 Healthcare Report. PE funds are regularly searching for a home to deploy this capital and physician practices are a common target.
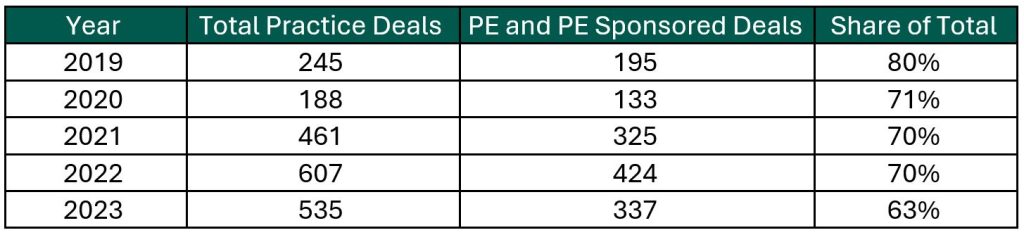
Source: Irvin Levin, 2024 Health Care Services Acquisition Report
Source: Irvin Levin, Healthcare M&A Quarterly Reports
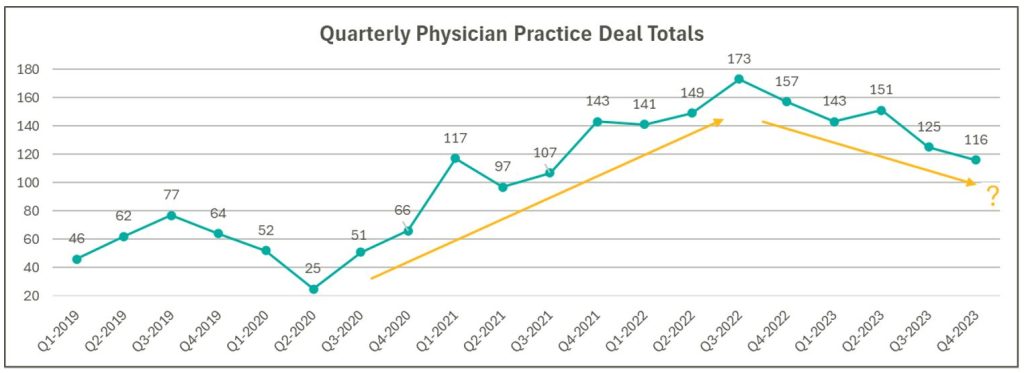
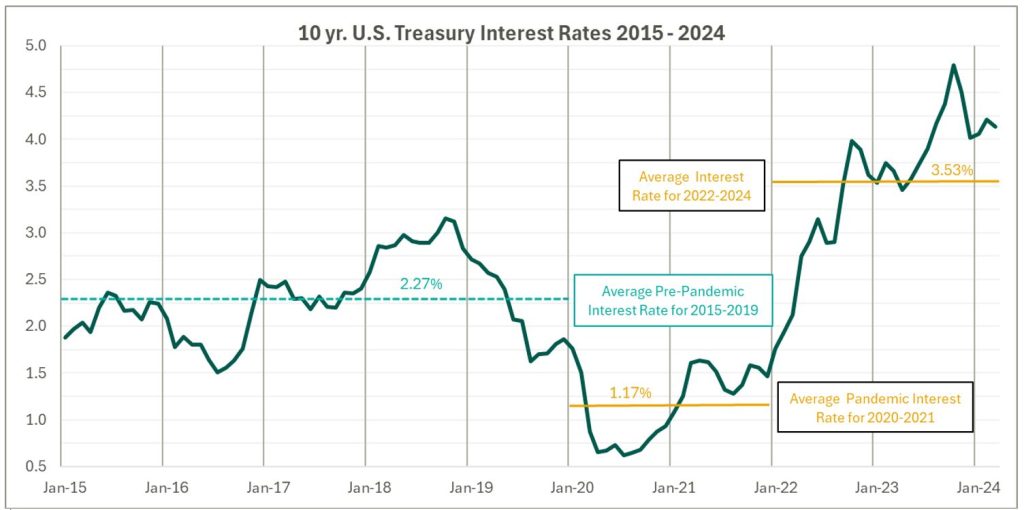
High Interest Rates: As the pandemic hit, fiscal stimulus and loosened monetary policy led to ultra-low interest rates relative to historical norms and spurred transaction activity. Interest rates began to materially rise throughout 2022, challenging overall transaction activity in the latter part of 2022 and during 2023 as access to capital tightened and the cost of capital increased. The below chart presents interest rates over the period as measured by the 10-year U.S. treasury.
Despite higher rates, transaction activity for physician practices has remained robust relative to pre-pandemic levels. However, there are signs that interest rates are having a lagged effect on deal volume considering the recent downward trend from Q3 2022 through Q4 2023 as observed in the above chart. While this does not necessarily mean that we should expect deal volume to revert to pre-pandemic levels, it does highlight that we have entered a new transaction environment. In this environment, the time to close deals lengthens as sellers digest lower valuation multiples and buyers increase scrutiny during due diligence given an uncertain future macroeconomic landscape. Contact VMG Health’s Financial Due Diligence team for details on how the changing tide is impacting the due diligence process.
At the start of 2024, interest rates remain elevated and volatile with an uncertain path to a normalized level, which continues to serve as a headwind for transaction activity. However, interest rates can change quickly, and the U.S. Federal Reserve has signaled that it will likely be appropriate to begin rate cuts at some point during 2024. Market participants have started anticipating rate cuts from this messaging, which could certainly serve as a tailwind throughout the remaining course of this year and into next.
Source: Federal Reserve 10 Year U.S. Treasury Market Data
Regulatory Transaction Oversight: Healthcare consumes a considerable amount of U.S. spending and is expected to continue increasing; CMS’ National Health Expenditure Accounts (NHEA) Healthcare projects healthcare spending to increase from approximately 18.3% of U.S. GDP in 2021 to 19.6% in 2031. Furthermore, it is an election year, with a current U.S. Presidential Administration keenly focused on the rising costs of healthcare. As a result, increased regulatory scrutiny has manifested itself over the ongoing consolidation across healthcare services, particularly within the physician practice space.
This heightened scrutiny is most recently evidenced by the Federal Trade Commission (FTC) suing U.S. Anesthesia Partners, Inc. (USAP), a prominent provider of anesthesia services in Texas, over an alleged “…anticompetitive acquisition spree to suppress competition and unfairly drive-up prices for anesthesiology services.” The FTC also hosted a workshop on March 5, 2024 to assess the public impact of private capital in healthcare. On that same day, the FTC, U.S. Department of Justice (DOJ) and U.S. Department of Health and Human Services (HHS) requested public comments on the effects of transactions involving PE, health systems, and payors on the healthcare providers and ancillary services space.
FTC Focus on Non-compete Agreements: It is not uncommon for physicians to a sign non-compete agreement upon joining a physician practice. The intent of a non-compete agreement, as well as the potential impact, are being hotly debated, with the FTC proposing a rule to ban non-compete clauses. A recent VMG article, Non-Compete Agreements: A Prevailing Quagmire provides details highlighting the arguments and broader implications of non-compete agreements and the proposed ban.
Overall interest in acquiring physician practices remains high, and we don’t expect that to change in the foreseeable future. The dynamics outlined above will likely dictate the path and volume of transactions throughout 2024 and beyond. To read more and stay informed as the year unfolds, please visit VMGHealth.com.
Centers for Medicare & Medicaid Services. Calendar Year (CY) 2024 Medicare Physician Fee Schedule Final Rule. Centers for Medicare & Medicaid Services website. Published November 2, 2023. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-final-rule
Centers for Medicare & Medicaid Services. CMS Finalizes Physician Payment Rule, Advances Health Equity. Centers for Medicare & Medicaid Services website. Published November 2, 2023. https://www.cms.gov/newsroom/press-releases/cms-finalizes-physician-payment-rule-advances-health-equity
Landi H. Physician groups decry finalized Medicare payment cuts as 2024 expenses rise. FierceHealthcare. Published November 3, 2023. https://www.fiercehealthcare.com/providers/physician-groups-decry-finalized-medicare-payment-cuts-2024-expenses-rise
American Medical Association. Only Cure for Medicare Payment Mess: Wholesale Reform. American Medical Association website. https://www.ama-assn.org/about/leadership/only-cure-medicare-payment-mess-wholesale-reform#:~:text=To%20put%20this%20into%20perspective,top%20of%20last%20year’s%203.8%25https://www.ama-assn.org/about/leadership/only-cure-medicare-payment-mess-wholesale-reform#:~:text=To%20put%20this%20into%20perspective,top%20of%20last%20year’s%203.8%25
VMG Health. 2023 Healthcare M&A Report. Published [publication date not provided]. https://vmghealth.com/2023-healthcare-ma-report/ https://vmghealth.com/2023-healthcare-ma-report/
PitchBook. Q4 2023 Healthcare Services Report. Published [publication date not provided]. https://pitchbook.com/news/reports/q4-2023-healthcare-services-report
Reuters. Fed’s Powell Set Election-Year Stage with Testimony on Rate Cuts, Inflation. Reuters website. Published March 6, 2024. https://www.reuters.com/markets/us/feds-powell-set-election-year-stage-with-testimony-rate-cuts-inflation-2024-03-06/
Centers for Medicare & Medicaid Services. National Health Expenditure Fact Sheet. Centers for Medicare & Medicaid Services website. Published [publication date not provided]. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/nhe-fact-sheet
Federal Trade Commission. FTC Challenges Private Equity Firm’s Scheme to Suppress Competition in Anesthesiology Practices Across the United States. Federal Trade Commission website. Published September [publication date not provided], 2023. https://www.ftc.gov/news-events/news/press-releases/2023/09/ftc-challenges-private-equity-firms-scheme-suppress-competition-anesthesiology-practices-across
McDermott Will & Emery LLP. Top Takeaways: FTC Hosts Workshop, Solicits Public Comment on Private Equity in Healthcare. McDermott Will & Emery LLP website. Published [publication date not provided]. https://www.mwe.com/pdf/top-takeaways-ftc-hosts-workshop-solicits-public-comment-on-pe-in-healthcare/
Aguirre I. Non-Compete Agreements: A Prevailing Quagmire. VMG Health website. Published [publication date not provided]. https://vmghealth.com/thought-leadership/blog/non-compete-agreements-a-prevailing-quagmire/https://vmghealth.com/thought-leadership/blog/non-compete-agreements-a-prevailing-quagmire/https://vmghealth.com/thought-leadership/blog/non-compete-agreements-a-prevailing-quagmire/