
Considerations in Structuring Physician Compensation-Per-WRVU Models
Rachel Linch
October 10, 2022
Effective January 16, 2024, Compliance Risk Analyzer has joined VMG Health. Learn more.
March 4, 2024
Written by Ben Minnis, Tyler Navarro, and Anthony Domanico
With significant changes to the Medicare Physician Fee Schedule (MPFS) in recent years and an aging physician population leading to potentially significant shortages of over 100,000 physicians by 2030,1 how organizations recruit and retain these key healthcare providers continues to evolve and become more competitive. As we hit the midway point of 2024’s first quarter, VMG Health’s experts have identified important trends in physician enterprise strategy that will impact the physician landscape in 2024 and beyond.
In today’s competitive recruitment landscape, organizations are innovating their approaches to attract and retain top physician talent. Beyond traditional compensation packages, which still include higher pay and signing bonuses in specialties facing shortages, institutions are prioritizing lifestyle enhancements like flexible scheduling and remote work options. Institutions are also promoting several non-traditional benefits and enhancements that attract and retain physicians:
The era of one-size-fits-all compensation models in multispecialty healthcare is coming to an end. As service lines within healthcare delivery settings evolve, so do their operational dynamics and corresponding compensation structures. Each service line has unique requirements, such as call coverage, sub-specialization (e.g., heart failure, ERCP), and supervision of advanced providers, among others. Attempts to enforce rigid standardization across various specialties within a physician enterprise are increasingly impractical and counterproductive in today’s complex landscape. Instead, organizations are recognizing the need to tailor compensation models to suit specific circumstances. Striking a balance between innovation and standardization is key for organizations seeking to optimize their compensation frameworks, as evidenced by VMG Health’s experience working with a variety of organizations and approaches.
Physicians are placing an increasing emphasis on achieving a healthier work-life balance. This shift in priorities is prompting healthcare organizations to reassess and refine their compensation packages to better align with the needs of modern physicians. Flexible scheduling options, including compressed work weeks or part-time arrangements, are gaining popularity because they allow physicians to better manage their time and commitments outside of work. Moreover, the widespread adoption of telemedicine has opened new avenues for physicians to practice medicine remotely, offering them greater flexibility in how and where they work. Additionally, paid time off (PTO) allowances are expanding to ensure physicians have ample opportunity for rest, relaxation, and personal pursuits.
A 2023 survey by Merritt Hawkins2 asked final year medical residents, “What is important to you as you consider practice opportunities?” Notably, 82% of respondents marked “lifestyle” as very important, indicating a clear preference for work arrangements that afford them the time and freedom to pursue personal interests and maintain a healthy work-life balance. Similarly, 80% of respondents cited the importance of having adequate personal time. Financial considerations remain unsurprisingly significant, with 78% of respondents emphasizing the importance of a good financial package. However, it is more and more evident that the pursuit of a fulfilling lifestyle and sufficient personal time are increasingly taking precedence in the minds of physicians when evaluating practice opportunities. This trend underscores the importance for healthcare organizations to adapt their compensation strategies to meet the evolving needs and priorities of today’s medical professionals.
The Centers for Medicare & Medicaid Services (CMS) have continued to delay implementation of proposed changes to the time-only definition of “substantive portion” of a split/shared E/M visit in the facility setting until December 31, 2024. Delays are due to a reportedly large backlash by facilities, with concerns over care team disruptions and issues with integrating a time-based rule into billing and EHR systems.
While VMG Health anticipates additional delays or even changes to the policy, it would be wise for organizations to prepare inpatient care models and related compensation models to ensure a proper plan is in place—or could quickly be implemented—when final rule changes do take effect.
In contemporary compensation structures, non-productivity incentives often include a substantial portion of compensation tied to high-quality metrics, ideally serving as a significant motivator and leading to better patient outcomes. While certainly not limited to a 2024 trend, forward-thinking organizations are continuing to leverage compensation design initiatives to bolster their ACO/CIN strategies, particularly those with health plans and/or substantial capitation risk within their payor contracts. As these organizations assume greater risk, compensation models can be tailored to distribute value-based earnings among physicians.
While physician shortages and increased demand continue to drive organizations to innovate compensation models and incentives, it’s crucial to operate within regulatory boundaries and adhere to laws governing healthcare practices. This point is underscored by recent cases, such as the one involving Community Health Network Inc., which agreed to pay $345 million to settle allegations of violating the False Claims Act by unlawfully submitting Medicare claims.3 The lawsuit alleged that Community Health Network overpaid specialists and awarded bonuses tied to referrals, ignoring warnings and providing false compensation figures. The settlement includes a five-year Corporate Integrity Agreement with HHS-OIG. The case originated from a whistleblower complaint filed in 2014. The government’s intervention underscores its commitment to combat healthcare fraud using tools like the False Claims Act.
In FY2022, the U.S. Justice Department collected $2.2 billion in settlements and judgments, the second-highest amount ever recorded in a single year. These statistics underscore the critical need for maintaining vigilance and compliance, particularly in an environment where regulatory scrutiny is significant.
Health systems are increasingly turning to advanced practice providers (APPs) as a strategic solution to address the pervasive challenges of physician shortages. Unlike for physicians, where organizations are competing nationally for talent, supply and demand trends for APPs are driven by local factors.
The rise of nurse practitioners, physician assistants, and other APPs is seen as a pragmatic response to the growing demand for healthcare services. These providers bring advanced education and training, offering a multifaceted approach to patient care that aligns with the evolving needs of modern healthcare. Organizations are looking to APPs for cost-effectiveness and because APP training programs are generating a higher number of graduates than medical schools. This allows organizations to fill needed vacancies quicker while considering changes to the care model that will drive down the total cost of care.
With competitive recruitment strategies and tailored compensation packages, health systems recognize the crucial role that APPs play in ensuring the continued delivery of high-quality and accessible healthcare services. This collaborative model enhances patient access, care coordination, and overall efficiency and fosters a supportive work environment where professionals can learn from one another and leverage their respective skills and expertise.
The trends shaping provider compensation in 2024 reflect a strategic response to ongoing challenges like physician shortages, regulatory constraints, and evolving workforce preferences. Physician enterprises will continue to face these challenges from a care model and compensation model perspective. VMG Health’s experts in physician enterprise strategy and compensation design can help your organization establish and refine your physician enterprise strategy to ensure your organization’s continued ability to recruit and retain top physician and APP talent.
1 Chakrabarti, R., et. al.(2021). The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. American Association of Medical Colleges. https://www.aamc.org/media/54681/download?attachment.
2 AMN Healthcare. (2023). Survey of Final Year Medical Residents. https://www.amnhealthcare.com/siteassets/amn-insights/surveys/survey-of-final-year-medical-residents-2023.pdf
3 United States Department of Justice. (2023). Indiana Health Network Agrees to Pay $345 Million to Settle Alleged False Claims Act Violations. https://www.justice.gov/opa/pr/indiana-health-network-agrees-pay-345-million-settle-alleged-false-claims-act-violations
February 23, 2024
Written by Jordan Tussy, CVA; Hunter Hamilton; and Vincent Kickirillo, CVA, CFA
Following the emergence of several oncology private equity (PE)–backed platforms in 2018, there has been an uptick of tuck-in acquisition activity in the oncology space, both by these PE-backed entities, as well as by other prominent public and corporate-backed oncology platforms. These platforms have targeted geographic expansion and economies of scale through strategic affiliations with practices and physicians.
In fact, a Harvard study published in JAMA Internal Medicine indicated that over 700 oncology practices had partnered with or had been acquired by a PE firm from 2003 to 2022. According to the study, this number represented approximately 10% of total oncology practice locations in the US.
While increased regulatory scrutiny and a more difficult funding environment have hampered overall physician practice transaction activity, several notable platform and tuck-in acquisitions have defined the recent environment for investment in oncology.

After a quiet couple of years from Pharos Capital Group’s Verdi Oncology, it was announced in November 2023 that the platform’s two practices, Nashville Oncology Associates and Horizon Oncology, had joined The US Oncology Network. Additionally, Verdi Cancer and Research Center of Texas, formed in August 2019, announced its closure in September 2023. With Verdi Oncology having been founded in March 2018 through the initial acquisition of Horizon Oncology, Pharos Capital Group’s assumed exit after nearly six years aligns with typical PE holding period expectations.

Perhaps most notable among recent transactions in the oncology space was the $2.1 billion acquisition of OneOncology from General Atlantic by TPG and AmerisourceBergen Corporation, which closed in June 2023. TPG will be the majority owner in the new joint venture, as AmerisourceBergen reportedly purchased a minority interest of approximately 35% for around $685 million in cash. TPG also has a one-year put option effective on the third anniversary of the deal closing. If exercised, this option would require Amerisource Bergen to purchase the remaining interest in OneOncology at a price equal to 19.0x the company’s adjusted EBITDA for the most recently ended 12-month period. AmerisourceBergen will also have a call option to purchase the remaining interest at the same price between the third and fifth anniversaries. Applying the 19.0x multiple to the transaction price of $2.1 billion would imply approximately $110 million of EBITDA for OneOncology today.
General Atlantic originally invested $200 million in OneOncology in September 2018 and held the investment for nearly five years. In that time, OneOncology has expanded considerably in both size and geography. The platform now includes 19 practices across 15 states with just under 1,000 providers. The structure is that of an affiliation model in which OneOncology charges a management fee and introduces partner practices to new ancillaries (e.g., oral pharmacy, laboratory services, radiation therapy) as well as lower drug-purchasing costs. Providers further benefit from a reduction in administrative burden and a resulting increase in clinical autonomy. In addition, OneOncology also has robust data analytics capabilities, which it utilizes to help define better clinical pathways, improve outcomes, and monetize the data.
Since the announcement of OneOncology’s acquisition by TPG and AmerisourceBergen in April, several additional practice partnerships have been announced, including the affiliation of Coastal Cancer Center and Pacific Cancer Care in May, Mid Florida Cancer Centers in November, and Pacific Cancer Medical Center, Maury Regional Medical Group, and Genesee Cancer and Blood Disease Treatment Centers in December. On January 12, 2024, it was announced that OneOncology had finalized a partnership with Huntsville, Alabama–based Clearview Cancer Institute, which—with 25 medical oncologist providing care across 13 clinics—was identified in the announcement as one of the five largest community oncology practices in the nation and the largest in Alabama.

After its recapitalization by Silver Oak Services Partners in October 2018, Integrated Oncology Network (ION) has continued its geographic expansion and now operates from more than 50 centers across 14 states in the US. Like OneOncology’s model, the independence of partner practices is also maintained under ION’s model, which, in addition to the preservation of clinical autonomy, offers to reduce the regulatory burden and increase access to the enhanced technology and resources of a larger network. ION specifically advertises its fully supported EHR and the immediate access its providers have to accurate data analytics. Most notably, in April 2022, ION announced the acquisition of California Cancer Associates for Research and Excellence (cCARE), an integrated cancer care network that provides medical oncology, radiation oncology, diagnostic imaging, and other ancillary services in the Fresno and San Diego markets. Furthermore, the platform expanded its cCARE operations with the September 2023 acquisition of High Desert Oncology of Victorville, California as well as the December opening of its new clinic in Riverside, California.

KKR-backed GenesisCare filed for Chapter 11 bankruptcy in June 2023, announcing that its US operations would be spun out from the broader enterprise. At the time of the announcement, David Young, CEO of GenesisCare, said, “The past three years have presented significant operational and financial challenges, requiring a comprehensive restructuring of the operations and balance sheet of the company.” No disruption of patient care was anticipated, and in November 2023, it was reported that GenesisCare had developed a reorganization plan to reduce its debt load by approximately $1.7 billion, down from the $2.0 billion it had at the time of filing. The US segment will continue to operate as a sister company to the businesses in Australia, Spain, and the UK, as the enterprise entertains interest from potential buyers.
According to bankruptcy filing documents, a number of winning bids for GenesisCare assets across the country have already been announced. Assuming these transactions close at the indicated prices (as defined in the respective purchase agreements), it would imply total cash proceeds of over $100 million. Furthermore, the sales of these 31 practices have an implied consolidated equity value of approximately $131 million.
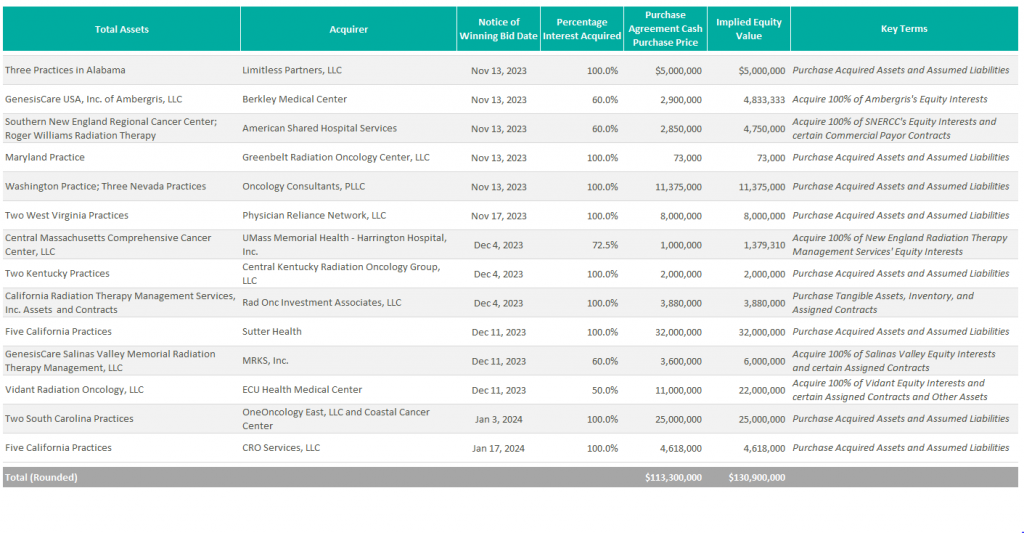
Additionally, it was announced in October 2023 that GenesisCare’s Orange County radiation oncology centers were acquired by UCI Health.

New to the scene is Oncology Care Partners (OCP). Backed by Welsh, Carson, Anderson, & Stowe’s healthcare platform, Valtruis, and partnering with oncology and cardiology care management provider Evolent Health, OCP opened its first two practices in Phoenix and Miami in January 2023 with the goal of advancing value-based care, particularly among Medicare Advantage patients. Based on the launch announcement of these first two practices, OCP appears to operate a hybrid model of practice partnership. The launch of its Arizona practice came in partnership with American Oncology Network, while its Miami-based medical group practice appears to have been an outright acquisition. Under both agreements, OCP says it will provide value for payors and at-risk primary care groups through the introduction of a new patient journey and digital tools to allow community providers to spend more time with their patients and reduce barriers to access. With the launch of its most recent location in Broward County, Florida in October 2023, OCP plans to continue expansion efforts across the country to further accelerate its value-based care initiatives.

McKesson’s The US Oncology Network (The Network) has also remained active expanding its footprint in California, New Mexico, and Kansas with the 2023 acquisitions of Epic Care, Nexus Health, and Cancer Center of Kansas, respectively. In April 2023, The Network also announced a strategic partnership with Regional Cancer Care Associates, a multispecialty oncology with more than 20 sites of service and over 60 providers throughout the Northeast. As previously mentioned, it was announced in the fourth quarter that Verdi Oncology’s Nashville Oncology Associates and Horizon Oncology had joined The Network as well. Under The Network’s affiliation model, the operational and clinical activities of its partner practices are converted to value-based care through greater focus on the negotiation of value-based contracts for revenue optimization, empowerment of practice transformation with proven solutions, alignment of GPO and payer contracts, and support for all oncology specialties. As of the most recent transactions, The US Oncology Network’s total provider count exceeds 2,400.

Previous stand-alone operator Cancer Treatment Centers of America (CTCA) was acquired by City of Hope in February 2022 for $364.4 million. At the time of its acquisition, the business operated three oncology hospitals located in Atlanta, Chicago, and Phoenix, as well as five outpatient facilities. On the one-year anniversary of the transaction, it was announced that CTCA was officially being re-branded to bear the City of Hope name at its facilities, further cementing the evolution of the organization into a national system.
In April 2023, American Oncology Network (AON) received a $65 million strategic growth investment from AEA Growth Partners “to help further AON’s goals of supporting community practices and improving the patient experience,” according to the Company’s press release. As a result of the investment, AEA Growth gained a minority interest in the business. AON opened Lone Star Oncology in Georgetown, Texas in June and announced the affiliation with Florida Oncology & Hematology in Safety Harbor, Florida in July. AON also ventured into urology through its affiliation with Triple Crown Urology on September 1. As a result of this transaction, AON’s platform now includes over 200 providers across 85 locations in 19 states and the District of Columbia. AON has a partnership model through which affiliated practices enter a management agreement and are charged a central services fee. Synergies realized through a partnership with AON are advertised as new revenue streams through centralized ancillaries, including oral pharmacy, clinical lab, and pathology as well as economies of scale with vendor services and drug pricing. With such revenue enhancements and cost reductions, providers can earn more than they otherwise might have as independent practices.
Most notable among AON’s recent transaction activity was the closing of a business combination with Digital Transformation Opportunities Corp., a special purpose acquisition company (SPAC), in September 2023. As a result of the transaction, AON began trading on the Nasdaq on September 21, 2023 under the ticker AONC. The transaction had an implied enterprise value of $497 million, with an implied TEV/Revenue multiple of 0.4x and an implied TEV/EBITDA multiple of 13.8x.

In November 2021, The Oncology Institute (TOI) was acquired by DFP Healthcare Acquisitions Corp., a SPAC, and became the first publicly traded oncology company. At the time of the acquisition, TOI’s pro forma enterprise value was $842 million. Underperforming initial expectations, the company ended 2023 with an enterprise value of approximately $148 million. To address these issues, TOI completed a corporate restructuring in Q2 2023 and has a strategic plan to eliminate cash burn and generate positive adjusted EBITDA by the end of 2024. According to their most recent earnings call, the company also plans to improve margins in legacy markets through expansion in capitated partnerships, radiation oncology, and clinical trials program. As part of this initiative, TOI acquired Southland Radiation Oncology Network in June 2023, which includes five radiation oncology clinics in the Los Angeles market. Despite the operational difficulties, The Oncology Institute remains the largest value-based care oncology operator in terms of lives served and revenue under value-based arrangement. To advance these efforts, The Oncology Institute acquires and employs the providers of its partner practices. The synergies it promotes include access to clinical trials, transfusions, and additional care delivery models more typically associated with the most advanced care delivery organizations.
Burdened with reimbursement headwinds and rising costs, it is anticipated that oncologists will continue to seek out strategic affiliations. Platforms such as OneOncology and The US Oncology Network offer an attractive alternative that allows physicians to maintain their independence while receiving the infrastructure and growth support of a large entity.
Furthermore, the long-term performance of major players in the oncology value-based care space remains to be seen, as does The Oncology Institute’s ability to achieve on its path to profitability in 2024.
Lastly, with the acquisition of OneOncology, ION is one of the last pureplay, PE-backed oncology platforms that has yet to recapitalize. Given Silver Oak Services Partners has held onto this investment for over five years now, it would not be surprising if there was a recapitalization of this platform within the next couple of years.
Silver Oak Services Partners LLC. (2023). Integrated Oncology Network acquires California Cancer Associates for research & excellence. PR Newswire. https://www.prnewswire.com/news-releases/integrated-oncology-network-acquires-california-cancer-associates-for-research–excellence-301530782.html
Integrated Oncology Network. (2023). Integrated Oncology Network announces High Desert Oncology joins cCare. PR Newswire. https://www.prnewswire.com/news-releases/integrated-oncology-network-announces-high-desert-oncology-joins-ccare-301933873.html
Integrated Oncology Network. (2023). Integrated Oncology Network announces cCare expansion with specialty clinic in Riverside, California. PR Newswire. https://www.prnewswire.com/news-releases/integrated-oncology-network-announces-ccare-expansion-with-specialty-clinic-in-riverside-california-302009492.html
Sebastian, D. (2023). KKR-Backed Radiotherapy Group GenesisCare Files for Bankruptcy. Wall Street Journal. https://www.wsj.com/livecoverage/stock-market-today-dow-jones-06-01-2023/card/kkr-backed-radiotherapy-group-genesiscare-files-for-bankruptcy-LIVUzBoTLS8Z2Z8qPcP9
GenesisCare. (2023). GenesisCare’s Plan of Reorganization Confirmed by Bankruptcy Court with Overwhelming Support from Voting Creditors. GenesisCare Newsroom. https://www.genesiscare.com/us/news/genesiscares-reorganisation-plan-confirmed-with-overwhelming-support-from-voting-creditors
UCI Health. (2023). UCI Health purchases GenesisCare radiation oncology centers. UCI Health News. https://www.ucihealth.org/news/2023/10/fountain-valley-radiation-oncology#:~:text=Acquisition%20expands%20access%20to%20world,cancer%20care%20in%20Orange%20County&text=Orange%2C%20Calif.,filed%20for%20Chapter%2011%20bankruptcy.
American Shared Hospital Services. (2023). American Shared Hospital Services Enters Into Agreement to Acquire 60% Majority Interest in Three Radiation Therapy Cancer Centers in Rhode Island. GlobeNewsWire. https://www.globenewswire.com/news-release/2023/11/20/2783147/0/en/American-Shared-Hospital-Services-Enters-Into-Agreement-to-Acquire-60-Majority-Interest-in-Three-Radiation-Therapy-Cancer-Centers-in-Rhode-Island.html
United States Securities and Exchange Commission. (2023). Form 8-K for American Shared Hospital Services. https://app.quotemedia.com/data/downloadFiling?webmasterId=101803&ref=317881267&type=PDF&symbol=AMS&cdn=1833bea1c9c3490a4573fbbc20a1fc5e&companyName=American+Shared+Hospital+Services&formType=8-K&formDescription=Current+report+pursuant+to+Section+13+or+15%28d%29&dateFiled=2023-11-21
Oncology Care Partners. (2023). Oncology Care Partners Launches First Three Locations, Bringing Patient Experience Focus to Cancer Care in Phoenix, Miami. PR Newswire. https://www.prnewswire.com/news-releases/oncology-care-partners-launches-first-three-locations-bringing-patient-experience-focus-to-cancer-care-in-phoenix-miami-301724825.html
Oncology Care Partners. (2023). Oncology Care Partners Launches Broward Location Expanding Value-Based Cancer Care in South Florida. PR Newswire. https://www.prnewswire.com/news-releases/oncology-care-partners-launches-broward-location-expanding-value-based-cancer-care-in-south-florida-301947441.html
American Oncology Network. (2023). American Oncology Network, a Rapidly Growing Network of Community-Based Oncology Practices, Receives Strategic Investment from AEA Growth. American Oncology Network News. https://www.aoncology.com/2023/04/28/american-oncology-network-receives-strategic-investment-from-aea-growth/
February 22, 2024
Written by Dylan Alexander, CVA and Gerrit Elzinga, CVA
As of January 2024, Definitive Healthcare reports that there are over 338,000 physician group practices in the United States. In an independent physician practice, shareholder physicians typically take home all earnings of their business and have discretionary expenses. The compensation package of the shareholder physicians negotiated during a transaction often differs from the compensation structure of the practice pre-transaction and should be taken into consideration in the valuation of a physician practice. An inverse relationship often exists between physician compensation and the valuation of independent physician groups. This means that higher post-transaction physician compensation results in less available earnings for the practice owners to sell, ultimately leading to a lower valuation for the physician practice. Post-transaction physician compensation structure plays a significant role in the value of physician practices.
There are many forms of physician compensation. Here are a few of the most common types:
Physician compensation levels vary from practice to practice. As previously mentioned, shareholder physicians typically take home all practice earnings; therefore, the post-transaction compensation structure will determine whether the subject practice has earnings or compensation to monetize in a transaction. Numerous factors determine whether physicians have compensation available to sell. Productivity and reimbursement are the main components for driving fee-for-service revenue at a physician practice. Practices with productive physicians, favorable reimbursement, and ancillary service offerings generate higher revenue, which results in increased profitability. Furthermore, practices that effectively leverage mid-level providers tend to have greater profitability than those that do not, as mid-level providers deliver many of the same services at a fraction of the cost. Expense management is key; a practice overburdened with operating expenses will be less profitable. For certain practices, historical physician compensation and its attributes may not leave meaningful earnings to sell.
Physician practices are most often valued utilizing three methodologies: income approach, cost approach, and market approach. The income approach considers the future earning potential of a physician practice and discounts the projected cash flows back to its present value. The value of a physician practice is sensitive to the total amount of physician compensation and how that compensation is structured. The greater the physician compensation, the lower the projected free cash flows will be. Ultimately, a high level of post-transaction physician compensation results in a lower valuation for the practice. Conversely, lower levels of post-transaction physician compensation create increased projected free cashflows. However, total compensation should be consistent with market levels. If the compensation structure is below market, there are sustainability risks associated with retaining and recruiting new physicians after the transaction. Setting physician compensation in line with the market for physicians with similar productivity can mitigate these risks.
The market approach compares an individual practice to similar physician practice transactions in the market through the application of an earnings multiple. Practice transactions often use the application of earnings before interest, taxes, depreciation, and amortization (EBITDA) multiples. It is important to note that EBITDA is calculated after taking into consideration the post-transaction structure for all providers. The multiple is determined based on a review of similar transactions in the marketplace, attributes specific to the practice, market factors, and on perceived risk of practice profitability amongst other factors. As illustrated below, physician compensation impacts the market approach similarly to the income approach—the greater the physician compensation, the lower the earnings for which to apply an earnings multiple.
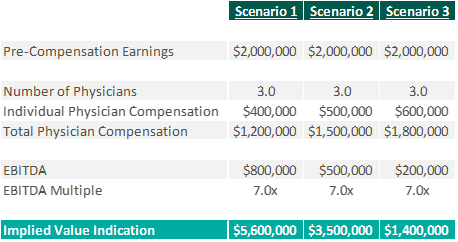
If too much physician compensation is sold, the market multiple may need to decrease to account for physician sustainability risk. Low levels of physician compensation in relation to productivity can lead to physician attrition.
The cost approach is an asset-based approach that analyzes an entity’s tangible and identifiable intangible assets. A level of post-transaction physician compensation that is consistent with the historical amounts or higher may eliminate positive future cash flows, causing the practice to be valued based on its assets versus earnings. It is not uncommon for practices to be valued using the cost approach due to the lack of attributes enabling them to monetize compensation while being consistent with market levels of compensation post-transaction.

Physician practices have the unique freedom to determine the services they provide, who provides those services, and how physicians can be compensated. There are multiple factors that determine the profitability of a physician practice, which directly impacts physician compensation. The amount of compensation and the way it is structured can have material impacts on the value of a practice, regardless of valuation approach. It is imperative to understand the link between post-transaction physician compensation and the fair market value of a physician practice for both buyers and sellers.
Definitive Healthcare. (2024). Number of physician group practices by state. Healthcare Insights. https://www.definitivehc.com/resources/healthcare-insights/number-physician-group-practices-by-state#:~:text=According%20to%20our%20database%2C%20there,them%20access%20to%20more%20patients
Kelleher, S. (2023). Understanding Physician Compensation Models. Health eCareers. https://www.healthecareers.com/career-resources/residents-and-fellows/understanding-physician-compensation
PayrHealth. (2022). Ancillary Services in Healthcare: Finding the Right Level for Your Practice. Managed Care Contracting Blog. https://payrhealth.com/resources/blog/list-of-ancillary-services-in-healthcare/
February 19, 2024
Written by Colin Haslett and Grayson Terrell, CPA
Healthcare transactions are known for their complex nature, given their rigorous regulatory compliance requirements, diverse revenue streams, intricate insurance and reimbursement policies, and significant capital requirements. Like a medical examination, financial due diligence evaluates the vital signs of a healthcare business, providing a comprehensive assessment of its financial health. By identifying potential financial risks and validating the company’s underlying valuation, due diligence helps to diagnose the current state of the business and predict its future health. No matter the size of the healthcare transaction, financial due diligence is a necessary element in the process. It provides valuable insights into the buy-side and sell-side, ensuring all parties clearly understand the financial aspects of the deal.
One important aspect of financial due diligence in healthcare transactions is the quality of earnings process, which focuses on adjusting or normalizing EBITDA. This process involves adjusting or removing the impact of any non-recurring or one-time items from EBITDA, providing a more accurate picture of the company’s true cashflows. Throughout this process, key facts about the company that could impact the company’s EBITDA may arise, highlighting the importance of thorough financial due diligence relative to the healthcare transaction. During the quality of earnings process, it is important to carefully examine the impact of various factors on EBITDA. Some potential examples include:
In addition to examining the impact of adjustments to EBITDA, the letter of intent (LOI) will include language outlining that the proposed transaction will be completed on a cash-free, debt-free basis. As such, another focus of due diligence is identifying the debt and debt-like items within the company’s financials. These items may include deferred revenues and compensation, outstanding legal proceedings and exposures, and accrued interest. Sometimes, these items are not included in a company’s financial statements, especially if they are on a cash-basis or are off-balance sheet. Furthermore, the LOI will state a normalized level of net working capital (NWC), agreed upon by the buyer and seller, needed to run the business post-transaction. Diligence procedures will often include an NWC analysis that ensures the buyer or seller is not allowing the targeted NWC to be set too high or low, which can be costly if the target levels are not met.
In conclusion, financial due diligence is not just a check-the-box exercise, but a critical process that mitigates risk and safeguards the likelihood of success for the transaction. Therefore, it’s an investment worth making. Adjustments to EBITDA made during the diligence process can often pay for the cost of diligence itself when the multiple of the transaction is considered. Neglecting to perform financial due diligence can have serious repercussions. Without a thorough understanding of the involved entity’s financial health, companies may overlook hidden liabilities, overestimate current and future earnings of the company, or underestimate the costs associated with integration.
February 13, 2024
Written by Ryan Mendez, Jack Hawkins, and Colin Park, CPA/ABV, ASA
The following article was published by Becker’s ASC Review.
The ambulatory surgery center (ASC) sector continued to evolve in 2023, reflecting a trend of steady growth, higher-acuity cases, and some changing regulations. 2023 featured continued consolidation through a combination of investment by prominent ASC platforms and acquisitions made by new entrants in the market.
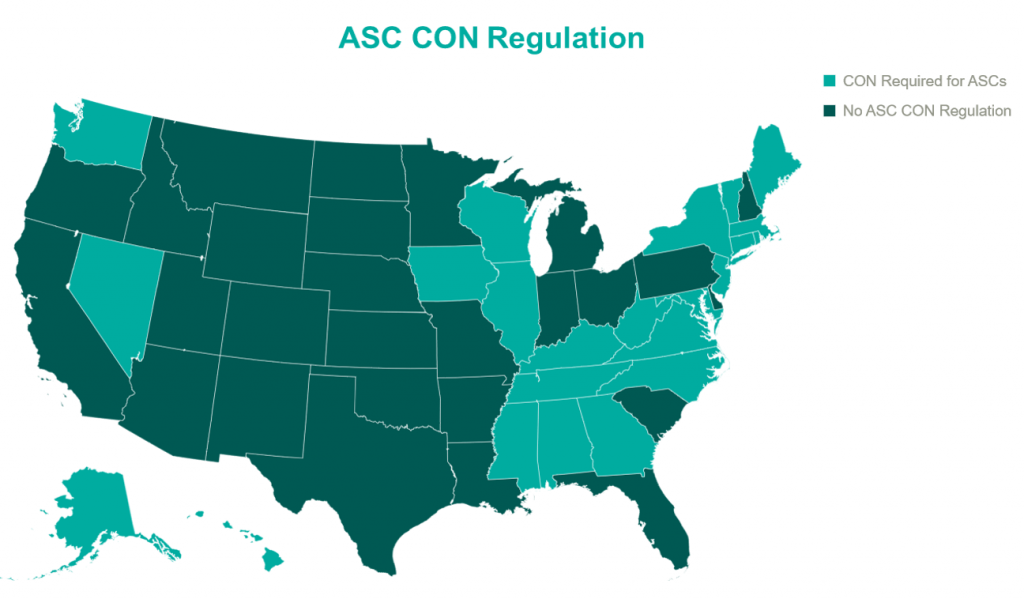
Higher acuity cases continued to decant to the outpatient setting, and with the Centers for Medicare & Medicaid Services (CMS) moving total shoulder arthroplasty to the ASC Covered Procedures List, we expect this shift to continue. In addition to these trends, 2023 saw significant changes in the regulatory landscape, particularly with the liberalization of Certificates of Need (CON) requirements for certain states. The changing of CON regulations is poised to further accelerate the development opportunities of ASCs, enhancing their ability to meet the increasing demand for outpatient surgical care. 2023 continued to solidify the ASC’s role as a dynamic force in healthcare, poised to meet the surging demand for efficient, accessible surgery.
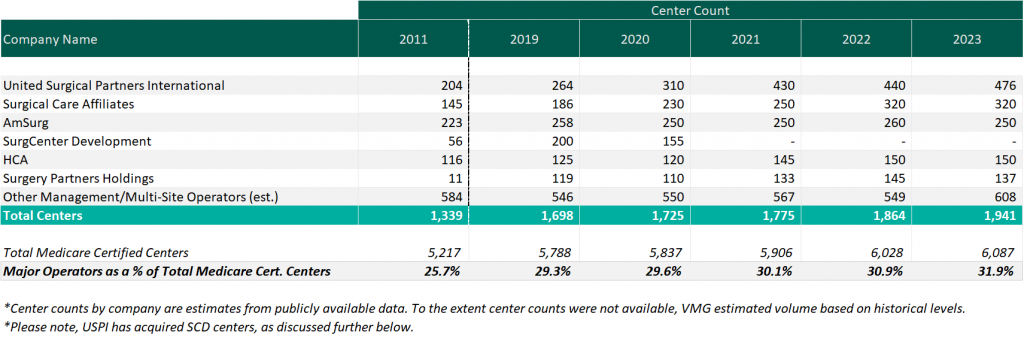
As of December 31, 2023, the largest operators (in terms of number of ASCs) are United Surgical Partners International (USPI), Envision Healthcare/Amsurg Corporation, and Surgical Care Affiliates (SCA), with ownership in approximately 476, 320, and 250 ASCs respectively. As noted in the chart below, the number of total centers under partnership by a national operator saw an increase from 2011 to 2023, growing from approximately 1,339 centers to 1,941 centers, which represents a compound annual growth rate of 3.14%. Additionally, the top five management companies have increased the number of centers under management by approximately 578 centers since 2011, which represents a compound annual growth rate of 4.85%. As management companies have increased in size, they can increasingly provide a greater level of strategic value by bringing greater leverage with commercial payors, enhanced management and reporting capabilities, and improved efficiency related to staffing, supplies procurement, and other general and administrative expenses.
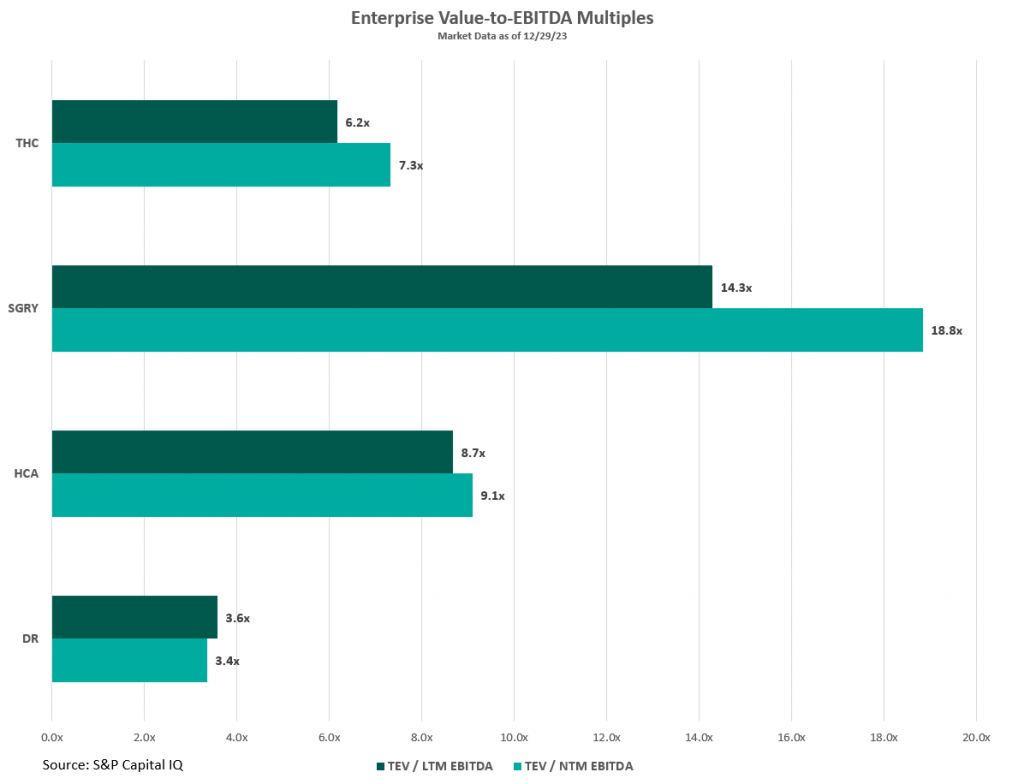
Public companies in the ASC market such as HCA Healthcare (HCA), Tenet Healthcare (THC), Surgery Partners (SGRY), and Medical Facilities Corporation (DR) offer insights into the ASC industry’s trends, challenges, and transaction data. These firms’ valuation multiples, illustrated in the figure below, serve as indicators of market valuation that are key to understanding the broader trends within the sector. Considering these multiples requires a nuanced approach, especially since larger organizations like HCA and THC have diversified operations beyond ASCs, which affect their market valuation and risk profiles. For example, HCA manages a large number of hospitals within its extensive healthcare services network, and THC’s ASC management platform, USPI, significantly impacts its profitability despite THC also operating numerous hospitals. To gain a comprehensive understanding of the ASC industry, it is beneficial to examine the detailed financial disclosures of these public companies. These include investor presentations and SEC filings, which offer a deeper insight into their performance and prospects than valuation multiples alone can provide.
For those interested in exploring the ASC industry further, including obtaining benchmarking information and analysis of ASCs across the United States, VMG Health’s Intellimarker is a valuable resource. The Intellimarker is an advanced, multi-specialty ASC benchmarking tool designed to facilitate a better understanding of ASCs’ relative financial and operational performance. Additionally, VMG Health’s Pulse on The Public Market provides coverage of various healthcare verticals in addition to the ASC sector.
In Q3 2023, Surgery Partners showcased a solid performance in the ASC sector, with surgical cases rising nearly 6% year –over year to over 172,000, after adjusting for divested facilities. This growth was driven by an emphasis on higher acuity cases and strategic acquisitions, as noted by Executive Chairman Wayne DeVeydt, culminating in $674.1 million in net revenue and $105.5 million in adjusted EBITDA for the quarter. The company experienced an uptick in total joint replacements, which increased by approximately 60% year –to date, supported by the recruitment of nearly 500 new physicians who specialize in musculoskeletal procedures into their centers. Despite facing challenges like anesthesia coverage and cost pressures, CEO Eric Evans is optimistic about the company’s long-term prospects, underlining its strategic focus on complex, higher-margin surgeries. Surgery Partners’ strategic acquisitions throughout the year have both bolstered its competitive position and broadened its geographical footprint and specialty mix, reinforcing its standing in high-growth markets and specialties.
During Tenet Healthcare’s Q3 2023 earnings call, the company highlighted its strong performance in ASC operations by its subsidiary, USPI. The ASC arm of THC reported a robust quarter with $370 million in adjusted EBITDA, a 16% increase from the same period in 2022, driven by a 7.9% rise in same-facility revenues and sustained margins. The subsidiary experienced notable volume growth in high-acuity service lines, including a mid-teens increase in total joint replacements, attributed to attracting high-quality physicians and leveraging increased patient demand for ambulatory surgery care. Additionally, THC expanded its ASC portfolio in Q3 by adding six new centers focused on higher-acuity orthopedic services in states like Nevada, Maryland, Texas, and Florida, featuring top musculoskeletal specialists. According to CEO Saum Sutaria, USPI’s aggressive expansion strategy includes over 30 centers in development, emphasizing high-value, specialized healthcare services. This expansion, part of a broader effort to advance site of service value-based care, aims to position USPI for sustained growth and profitability by tapping into high-growth, high-margin healthcare services and meeting patient demand for specialized ambulatory care.
In Q4 2023, HCA Healthcare reported a robust performance, with CEO Sam Hazen highlighting the strong demand across service lines and the improved operational efficiencies that led to a significant revenue increase to $17.3 billion. This performance, which surpassed expectations, was supported by a near 14% increase in adjusted EBITDA compared to the same quarter last year. This growth was driven by an 11% increase in same-facility revenue and improvements in operating margins, highlighting HCA’s ability to leverage increased revenue effectively. CFO Rutherford identified HCA’s ambulatory surgery division contributions to this success, demonstrating the company’s strategic focus on expanding its high-acuity service offerings and enhancing patient care through strategic acquisitions and network expansion.
During the 2023 Q3 earnings call, Medical Facilities Corporation demonstrated a strong financial performance, driven by strategic divestitures and a concentrated effort on core operations, resulting in a 7.4% rise in facility service revenue to $104.6 million. The executives highlighted significant operational improvements, including a 13.7% increase in EBITDA, attributed to enhanced efficiency and cost-saving strategies. Interim President Jason Redman noted that the increased performance was largely due to case mix, but that surgical case volumes also increased by 1%. Medical Facilities Corporation saw three of their surgical hospitals recognized for excellence in joint replacement, emphasizing the strategic shift towards managing higher-acuity cases in outpatient settings.
The trend of shifting higher-acuity procedures from inpatient or Hospital Outpatient Department (HOPD) settings to ASCs continued to grow throughout 2023. Specialties like cardiology, orthopedics, and advanced spine procedures increasingly marked their presence in ASCs. Throughout the year, many ASCs doubled down on their high-acuity procedures to drive revenue growth. Annu Navani, founder of Comprehensive Spine & Sports Center in Campbell, CA, elaborated: “The growth in orthopedics, spine and pain has been steady and will remain so. These are safe specialties, as the need is always there and will continue to thrive…” It is more than just a concept, as Surgery Partners CFO, David Doherty, provided some insight into how higher-acuity cases have spurred growth during the company’s Q3 earnings call. Doherty noted, “On a same-facility basis, total revenue increased 14.2% in the third quarter, with case growth at 2.9%. Net revenue per case was 11.0%, higher than last year, primarily driven by higher-acuity procedures.” This continued shift towards higher-acuity procedures being performed in ASCs is a clear indicator of the sector’s adaptation and growth, meeting the evolving demands of healthcare while offering efficient and cost-effective solutions for complex medical needs.
In 2023, ASC operators focused on both organic growth within their existing high-acuity specialties and actively pursued M&A opportunities as a key strategy to expand their footprint. During Surgery Partner’s Q1 earnings call, CEO Eric Evans noted that, “With an increase in the share of orthopedic and cardiac procedures moving into lower-cost, high-quality, short-stay surgical facilities, we are considering all options to capture our fair share, including sourcing and managing a robust M&A pipeline…”
Similarly, during THC’s Q3 earnings call, CEO Saum Sutaria, reiterated that THC is committed to scaling their ASC portfolio: “During the quarter, we added six new centers, the majority of which were focused on higher-acuity orthopedic services.” These developments illustrate the sector’s dynamic response to changing healthcare demands, positioning it for sustained growth and wider service reach as more high-acuity cases continue to shift to the ASC setting.
CMS noted in its fact sheet that, “in addition to finalizing payment rates, this year’s rule includes policies that align with several key goals of the Biden-Harris Administration, including promoting health equity, expanding access to behavioral health care, improving transparency in the health system, and promoting safe, effective, and patient-centered care. The final rule advances the Agency’s commitment to strengthening Medicare. It uses the lessons learned from the COVID-19 PHE to inform the approach to quality measurement, focusing on changes that will help address health inequities.”
CMS finalized the addition of 37 surgical procedures to be added to the ASC CPL for CY 2024, outlined in the table below. These include 26 dental codes that were included in the proposed rule, and 11 surgical codes that were not included in the proposed rule—most notably total shoulder arthroplasty. These codes correspond to procedures that have little to no inpatient admissions and are widely performed in outpatient settings.
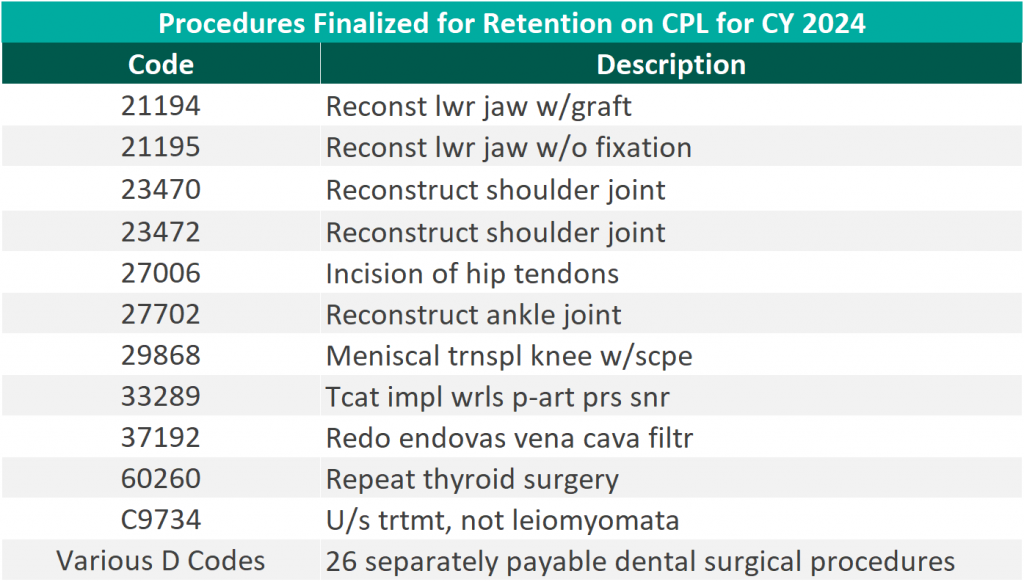
“We thank CMS for heeding our request to move additional surgical procedures—including total shoulder arthroplasty—onto the ASC payable list. Doing so benefits both Medicare beneficiaries, who now have a lower-cost choice for the care they need, and the Medicare program itself, which will save millions of dollars as volume moves to the high-quality surgery center site of service.” – Bill Prentice, Chief Executive Officer, ASCA
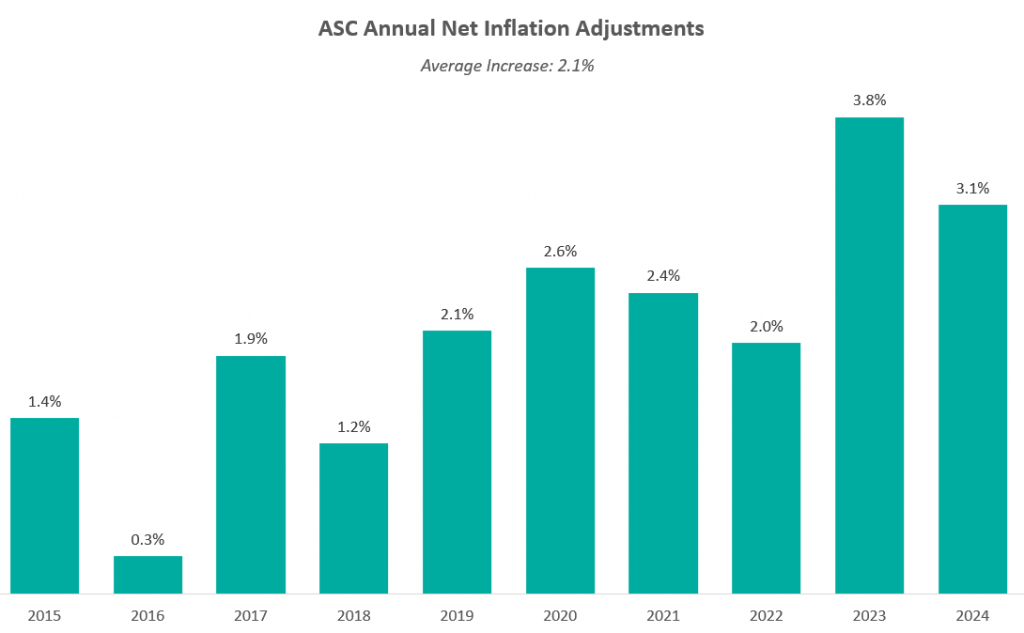
On November 1, 2022, the Medicare reimbursement fee schedule for ASCs in 2023 was finalized by CMS. Consistent with previous years, For CYs 2019 through 2023, CMS will update the ASC payment system using the hospital market basket update, rather than the Consumer Price Index for All Urban Consumers (CPI-U). CMS published the 2022 ASC payment final rule, which resulted in overall expected growth in payments equal to 3.8% in CY 2022. This increase is determined based on a hospital market basket percentage increase of 4.1% less the multifactor productivity (MFP) reduction of 0.3% mandated by the ACA. The 3.8% growth in payments represented the largest increase in projected payments year over year and was a direct result of the increase in labor, supplies, and other cost pressures seen over the last year.
Moreover, CMS released the ASC payment final rule for CY 2024 on November 2, 2023, resulting in overall expected growth in payments equal to 3.1% in CY 2023. This increase is determined based on a projected inflation rate of 3.3% less the MFP reduction of 0.2% mandated by the ACA. This is an increase of 0.3% from the proposed rule. Many healthcare industry leaders think the recent payment hike is too small given the intense cost pressures on hospitals and ASCs. How ASCs manage in today’s changing economic climate will be closely watched in the coming years
The chart below presents a summary of the historical net inflation adjustments for CY 2015 through CY 2024. The annual inflation adjustments are presented net of additional adjustments, such as the MFP reduction, outlined in the final rule for the respective CY. The CY 2024 inflation adjustment is slightly lower than the increase observed last year, although it continues to be elevated compared to the adjustments observed prior to 2023 largely driven by labor and supply cost pressures.
The table below reflects a summary of the estimated Medicare ASC payments for 2023 and 2024 for the top 10 CPT codes performed in ASCs in 2023. As noted below, the estimated 2024 payments by Medicare for the top 10 CPT codes from 2023 are projected to remain relatively flat overall, though there are some notable changes at the individual CPT level, including large decreases to three spinal/neuro stimulator codes.
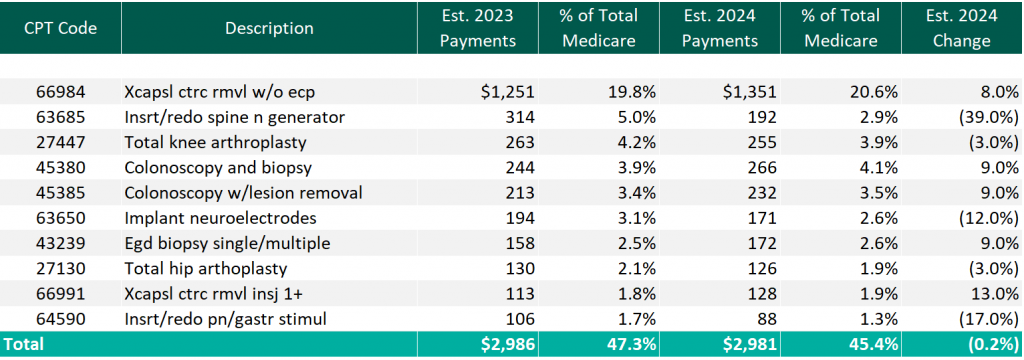
CMS has projected total ASC payments in 2024 to increase to approximately $7.1 billion, an increase of approximately $207 million compared to estimated CY 2023 Medicare payments.
In 2023, we saw the continued consolidation of the ASC market with individual transactions by prominent, large-level ASC platform players and M&A activity at the lower-middle-market level with a newly founded, private equity (PE) backed ASC development management company acquiring two centers to begin its platform. Although the industry continues to consolidate, as of 2023, approximately 68% of ASC facilities remain independent, leaving room for further consolidation at the individual-facility level.
The ASC market has seen a continued trend of intentional PE activity with interest in ASCs in recent years, most often tied to related physician practice portfolio companies. Driven by favorable tailwinds, this type of investment in ASCs allows PE investors to capture additional revenue streams related to their physician practice investments. PE interest in an ASC strategy outside of a physician practice portfolio company has also increased recently. Based on data from PitchBook’s Q3 2023 Healthcare Services Report, the ASC industry saw six trackable PE deals through September 30, 2022. These deals were mostly add-on investments, with one deal being a growth investment. PE total deal activity in the ASC space has remained fairly consistent over the last five years, though 2023 notably marks the first time since 2020 when no platform PE deals were tracked through PitchBook’s report. However, October 2023 saw the announcement of a PE-backed ASC platform.
In October 2023, a newly founded, multispecialty ASC development and management company, SurgNet Health Partners, Inc. (SurgNet), announced the acquisition of two ASCs in Michigan and Ohio. SurgNet is newly backed by Fulcrum Equity Partners, Leavitt Equity Partners, and Harpeth Capital. A $50 million equity check was syndicated to launch the platform, and presumably, additional investments will follow to support further investments. SurgNet, together with its equity partners, is expected to rapidly expand in the outpatient surgery market through aggressive growth strategies, including acquisitions, de novo ventures, and effective center management.
On February 9, 2023, United Musculoskeletal Partners (UMP) partnered with two orthopedic practices based in Dallas-Fort Worth. All-Star Orthopaedics, with four clinic locations, and OrthoTexas Physicians and Surgeons, PLLC, operating five clinics and one surgery center, were both acquired by the UMP platform. In August, UMP expanded this partnership by acquiring an ortho-focused surgery center, Pinnacle Orthopaedics, in an add-on LBO transaction.
In May 2023, The Office of Health Strategy (OHS) approved two settlement agreements allowing Hartford HealthCare (HHC) to acquire two outpatient surgical centers in Connecticut. On May 12, 2023, Surgery Center of Fairfield County, a subsidiary of HCA Health, was acquired by HHC, for an undisclosed amount. Further, in October 2023, HHC acquired Lichfield Hills Surgery Center, also for an undisclosed amount.
Covenant Physician Partners expanded its ASC footprint with the merger of its St. Vincent Eye Surgery Center and Wilshire Center for Ambulatory Surgery, adding an additional facility for surgeries.
On September 18, 2023, Unifeye Vision Partners (UVP), a management and support services company with an ophthalmology and optometry practice network including 13 ASCs, announced the acquisition of Insight Vision Group, a comprehensive eyecare platform in California. Insight Vision Group is made up of 10 clinics and two multi-specialty ASCs. UVP was active in the M&A space earlier in the year, acquiring Premier Surgery Center of Santa Maria, through an LBO for an undisclosed amount.
Surgery Partners further expanded its reach in September 2023, with the announcement of the acquisition and partnership with NorCal Orthopedic Surgery Center in San Ramon, CA. The center, an out-of-network ASC originally comprised of nine separate operating entities along with 25 physician partners, was advised by Merrit Healthcare Advisors in structuring the merger of the nine entities into one ASC to then be sold to Surgery Partners.
TriasMD, the parent company of DISC Surgery Centers and another musculoskeletal management company, declared its acquisition of Pinnacle Surgery Center in October 2023. This strategic move extends DISC’s data- and evidence-driven ASC model into Northern California, marking the second acquisition within the past six months. TriasMD previously acquired Gateway Surgery Center in Santa Clarita in February.
In November 2023, Regent Surgical Health acquired majority ownership in Oregon Surgical Institute (OSI), expanding a joint venture partnership that started in 2016. Notably, OSI was the northwest US’ first ASC to focus on complex spinal and total joint replacement cases. Regent COO Jeff Andrews said, “Our evolved partnership was made possible by the trust OSI’s leadership team has placed in us, and this will bolster both value and access by strengthening OSI’s position as a home for the growing list of procedures being delivered through ambulatory surgical centers nationally.” This development highlights the continued emphasis on pushing more complex cases to the outpatient setting through health system joint venture partnerships.
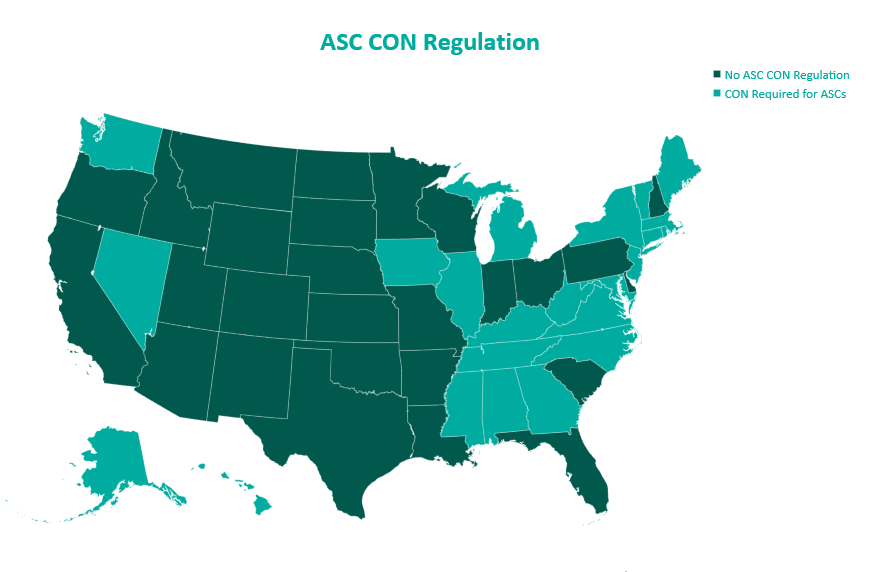
In 2023, the landscape of Certificates of Need (CONs) for ASCs underwent notable changes. South Carolina led the way with significant reform, eliminating CON requirements for most health facilities, including ASCs. North Carolina amended its CON law, reflecting a trend toward liberalizing these regulations. North Carolina’s modifications to its CON law specifically targeted easing the process for ASCs and certain medical facilities by adjusting the threshold for review. By raising the financial thresholds for mandatory review, ASCs can undertake significant investments in innovative technologies, expansions, or renovations without the need for a lengthy CON application and review process. The complete repeal of ASC CONs in North Carolina is expected in the coming years. In parallel, Mississippi and Georgia engaged in legislative actions to reevaluate their CON laws as well. Mississippi put forward a provision that would allow Hospitals to establish single-specialty ASCs without the requirement of a CON. Georgia proposed a bill that would eliminate CON requirement for hospitals and establish a unique healthcare service licensure process. With a potential domino effect that could sweep through many states, these regulation changes are important to keep an eye on in the coming years. The relaxation of CON laws may foster growth in the ASC sector with new center development, with more states likely to follow suit in the future, potentially leading to increased access to ASC services and further transformations in healthcare delivery and facility expansion.
The ASC sector experienced significant growth in 2023, driven by factors like industry consolidation, continued shift of care to outpatient settings, and new revelations in the regulatory environments. Key players expanded their operations, reflecting an overall increase in the number of centers managed by national operators. Higher-acuity cases continue the shift into outpatient settings as more procedures are added to the ASC Covered Procedures List. CMS’ policies and reimbursement rates played a crucial role in shaping the sector alongside the evolving landscape of CON regulations. Overall, the ASC market in 2023 demonstrated resilience and adaptability, positioning itself for continued growth and a more significant role in healthcare delivery.
September 28, 2023
Written by Christian Lynch and Chance Sherer, CVA
Ambulatory surgery centers (ASCs) continue to be the target of health systems, physicians, and financial investors due to their straightforward business model and ability to align with physicians. As more high-acuity, high-reimbursing procedures transition to the outpatient setting, ASCs will become increasingly attractive for investment and will further cement their status as a preferred, low-cost surgical setting. Given the considerable attention from potential investors, it is crucial to understand how value is measured, how that value is derived, and the common terms used to describe value.
To convey value, market participants often speak in terms of “multiples.” A multiple is simply a company’s enterprise value divided by an industry-specific metric. Multiples are used due to their simplicity and ability to compare subjects to industry peers without the need for complex analyses. Although multiples within healthcare can be based on many different metrics, such as number of beds, revenue, covered lives, panel size, etc., ASCs are most discussed in terms of EBITDA multiples.
EBITDA, defined as earnings before interest, taxes, depreciation, and amortization, generally approximates a center’s cash flow, and by extension, its profitability. By calculating earnings before non-cash charges, such as depreciation and amortization, EBITDA represents earnings available to shareholders better than net income. Additionally, excluding interest expense removes the effect of capital decisions, whereby shareholders decide to finance purchases with debt or purchase equipment outright. Due to the discretionary nature of utilizing debt instead of cash, removing the impact of such decisions makes EBITDA an easily comparable metric between industry participants.
Understanding EBITDA and its benefits provides a clearer picture of multiples and their meaning. For example, a multiple of 8x EBITDA means the target ASC can be wholly acquired for a sum equal to eight times its EBITDA. Despite the prevalence and simplicity of EBITDA multiples, there are a few significant pitfalls to be aware of.
First, it is important to recognize that EBITDA multiples are often discussed in terms of “implied” multiples rather than “applied” multiples. Put another way, the final transaction value is typically determined through a detailed analysis of the subject ASC’s historical and projected financial performance. This value is then divided by EBITDA to arrive at an implied multiple.
Investors and valuation professionals are concerned about the ultimate distributions received from an investment in an ASC and the associated risk/return. The distributions are assessed through a discounted cash flow analysis where future earnings are projected and discounted back to present-day dollars using a discount factor. The sum of these discounted cash flows is then used to estimate the value. This analysis allows for the consideration of many idiosyncratic factors relevant to the subject ASC, such as size, geography, capacity, specialty/case mix, payor mix, staffing and supply expense growth, capital requirements, and many other factors.
Conversely, simply applying a market multiple to EBITDA will give an indication of value but may not accurately reflect the specific factors of the subject ASC. Given the intricate analysis used to determine value, it is clear why ASC transactions at the control level do not all occur at the same multiple; one center may be valued at a 7.3x implied EBITDA multiple, and another may be valued at an 8.2x multiple.
Buyers and sellers must understand the range of EBITDA multiples in the market to ensure the analysis produces an appropriate result. If the implied multiple lies outside the market range the discounted cash flow analysis will provide an explanation as to why.
To fully understand an implied EBITDA multiple is it critical to know the EBITDA by which the multiple is calculated. As shown in the table below, the implied EBITDA multiple of ASC value can be expressed using several different types of EBITDA; however, the most common are historical, normalized, and projected. Historical EBITDA represents the actual earnings of the center in the prior 12 months. On the other hand, normalized or adjusted EBITDA represents earnings after adjusting revenues and expenses to depict what a normal past 12 months of operations would have looked like.
Typical adjustments include the removal of one-time expenses and revenues, transaction adjustments for related-party arrangements (i.e., management agreements, billing fees, rent expenses), and adjustments for the timing of certain revenues and expenses that are over-represented or under-represented in the examined historical period. Lastly, projected EBITDA represents the expected next 12 months of earnings after normalization. It may account for many specific factors, but commonly it varies from normalized EBITDA due to expected changes in case volume.
Using different types of EBITDA can have a material effect on multiples. For example, after removing certain nonrecurring expenses, a center’s normalized EBITDA might be $100,000 higher than the historical level. As a result, a control-level value indication of $10,000,000 would produce a multiple of 8.3x based on historical EBITDA, whereas using normalized EBITDA would imply a multiple of 7.7x.
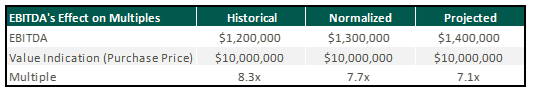
Though implied multiples are often discussed in terms of normalized or projected EBITDA, sellers should be cautious when hearing rumored valuation multiples among their peers. A possible disconnect between the various indications could distort the view of how ASCs are valued.
While it is beneficial to understand the general market ranges for ASC transaction multiples, an extensive assessment of the specific facts and circumstances of any singular center is required to determine its precise value. This valuation requires detailed knowledge of the operations and financial performance of the ASC from both a historical and future perspective. To determine an accurate valuation range for a center, buyers and sellers commonly engage the services of qualified advisors, such as VMG Health, who have extensive experience in ASC valuation.
September 21, 2023
Written by Josh Miner, Savanna Ganyard, CFA, and Taryn Nasr, ASA
The Ambulatory Surgery Center (ASC) market is a fast-growing sector of healthcare that is attracting considerable interest from private equity (PE) funds across the country. The following outlines the current state of the market as well as key factors driving ASC market growth and attracting PE investment.
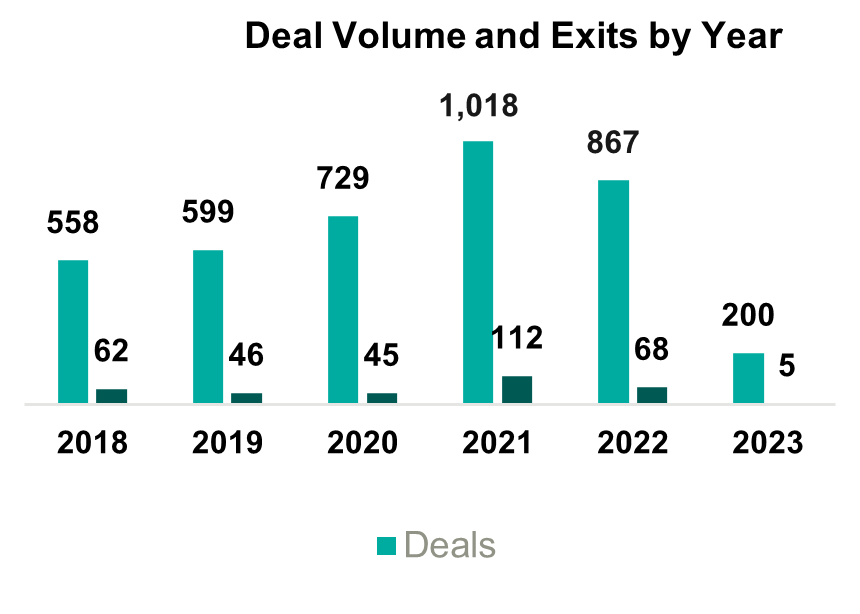
2021 saw the most PE-related healthcare transactions in history, with an estimated 1,018 transactions occurring throughout the year. During the first quarter of 2023, transaction activity slowed from the pace set in 2021, primarily due to macroeconomic factors including inflationary pressures, rising interest rates, and higher labor costs. Additionally, rising interest rates and tight credit have increased the cost of debt leading to a reduction in leverage of one to one-and-a-half turns. Uncertainty surrounding the bank debt market has led PE investors to turn to private credit and other deal strategies. These strategies include searching for smaller deals where securing financing may be easier or targeting add-ons that are small enough to purchase without debt.
Despite the recent slowdown in activity, it is likely that the deal volume will rebound as macroeconomic uncertainty eases, but, in the short term, PE firms will likely continue to target smaller platform deals and add-ons. These transactions will likely involve independent targets, as other institutional investors may not attempt an exit in the current economic conditions.
The ASC market was recently sized at $84 billion in 2020 and is projected to grow at a compounded annual growth rate (CAGR) of 3.9% to $131 billion by 2031. The industry is highly fragmented with 70% of ASCs independently owned and the remaining owned by larger conglomerates. Over the past several years, PE ownership in the ASC space has steadily increased. Two of the largest players in the industry, AmSurg and Surgery Partners, have PE ownership. Other major ASCs with PE ownership include Covenant Physician Partners, EyeCare Partners, Gastro Health, GI Alliance, HOPCo, PE GI Solutions, and Value Health. Notably, Bain Capital’s $3 billion leveraged buy-out (LBO) of Surgery Partners in 2017 remains the largest deal completed in this space.
The expected growth in the ASC industry is driven by numerous factors including a shift towards lower cost procedures. On average, patients save $684 per procedure at an ASC as compared to a hospital based on a 2021 report from UnitedHealth Group. Specifically, orthopedics is a growth area driven by cost savings. On average, ASCs reduced the cost of orthopedic procedures by 17% to 43%. These cost savings at an ASC lessen the burden on the patient and help boost margins in an ASC setting. As a result, orthopedics continues to be a popular specialty for investors pursuing an ASC strategy.
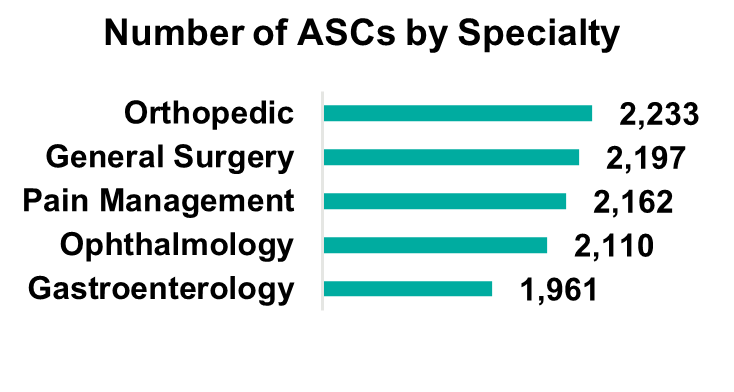
Orthopedics remains the most popular specialty, but gastroenterology, pain management, and ophthalmology make up large portions of the market. Notably, cardiology has become the fastest-growing specialty as ASCs invest in technology and higher acuity procedures continue to move to the ASC setting. The demand for cardiology is driven by an aging population and the level of cardiovascular disease in U.S. adults (e.g., half of all U.S. adults have cardiovascular disease). While cardiology is currently primarily a hospital-based specialty, with 70% of cardiologists employed by hospitals, as this specialty moves into ASCs there is a unique opportunity for PE firms to secure a foothold in a fast-growing segment.
On January 31, 2023, Lee Equity Partners (LEP) completed a buyout of the Cardiovascular Institute of the South (CIS) for an undisclosed amount (of note, LEP deals typically range from $50 to $150 million in equity). CIS has 21 locations across two states and employs over 60 physicians. This deal represents one of the larger buyouts of an ASC in recent memory and illustrates the growth of cardiology as a specialty in ASCs.
As more cases and specialties shift to an ASC setting, there is an increasing patient demand for multi-specialty ASCs. Patients are seeking convenience in the ability to receive treatment for a multitude of treatments in one place. The number of multispecialty ASCs is forecasted to expand at a 4.3% CAGR, outpacing general ASC market growth.
These industry characteristics coupled with the PE industry outlook should continue to drive transactions within this space, specifically among the 70% of independently owned ASCs. Due to recent macroeconomic factors, we expect PE firms to continue to pursue smaller add-on deals aimed at consolidating several ASCs in an area. These types of transactions allow PE firms to capitalize on industry trends, optimize cost-cutting opportunities, and generate attractive returns. On the other hand, these transactions are also attractive to independent and physician-owned ASCs due to the benefits of a larger growth infrastructure which can leave more time for physician owners to focus on patient care.
ASCs can offer cost savings and convenience to consumers without sacrificing quality of care. Due to increasing demand, the number of specialties, and the ability to perform high-acuity procedures, the ASC market is projected to grow steadily over the next decade. Market growth, combined with the availability of investment opportunities due to the fragmentation of the market, will continue to attract PE investment. As macroeconomic conditions become less uncertain, it is likely that PE investment will continue to rebound to historical levels in the healthcare industry. Furthermore, the many attractive qualities of the ASC industry should draw investment in the space.
August 28, 2023
Written by James Tekippe, CFA, Michael Schenck, and Ryan Diver
The following article was published by Becker’s ASC Review.
The No Surprises Act was a landmark piece of legislation aimed at protecting patients from unexpected medical bills. Although the law is a significant step forward for patient protection, it has resulted in a significant increase in financial support requests from anesthesia providers who serve patients at ambulatory surgery centers (ASCs). This article will outline the hallmarks of the act, its impact, and the operational and compliance considerations for ASCs that need to implement coverage arrangements with their anesthesia groups.
Prior to the No Surprises Act, patients who unintentionally received care from an out-of-network provider could potentially have received a “surprise medical bill” from a facility or provider. This occurred in emergency room situations where the patient had no ability to select the emergency room, physician, or ambulance provider. Additionally, surprise bills resulted from services provided at an in-network facility for a patient but from an out-of-network provider. This was common for services provided by anesthesia, first assist, and radiology providers.
Additionally, healthcare costs and pricing information were often difficult to obtain prior to receiving treatment, and patients frequently faced challenges in understanding the cost implications of their healthcare choices. Moreover, billing disputes between healthcare providers and insurance companies often left patients caught in the middle. Consequently, surprise medical bills could result in higher fees for patients in a couple of ways. First, higher cost sharing between health plans and patients, with most patients having to pay a higher co-pay for out-of-network services. Second, many providers would balance bills, which allowed “the out-of-network provider [to] bill consumers for the difference between the charges the provider billed, and the amount paid by the consumer’s health plan.”
Due to these circumstances, the No Surprises Act was passed as part of the Consolidated Appropriations Act, 2021 and began taking effect on January 1, 2022. Now after a patient receives care, the healthcare provider will verify the patient’s insurance and determine if they are in-network or out-of-network. If the patient receives care from an out-of-network provider at an in-network facility, the patient is only responsible for their in-network cost-sharing amount, such as deductibles, co-pays, or coinsurance. The provider will then bill the insurance for their services. After the insurance company processes the provider’s claim, the patient will then be billed for their responsibility for the in-network cost-sharing amounts. If there is a dispute between the provider and the insurance company regarding reimbursement for out-of-network services, the provider and insurance company may engage in the independent dispute resolution (IDR) process, where an independent arbiter reviews the case and determines the appropriate payment.
The implementation of the act has caused tension between providers and insurers. Prior to the act, many providers had relied on balance billing to generate revenue. Now, not only is this practice illegal in certain scenarios, but insurance companies are typically only willing to pay something near the qualified payment amount (QPA), which is the median rate for those in-network services for the given geographical area. This can neglect crucial factors and can be very different from the amount they were used to receiving. This has resulted in numerous providers and payers entering negotiations and the IDR process.
Given the reduction in billings that some provider groups may be experiencing because of the No Surprises Act, anesthesia groups with coverage arrangements with ASCs have found themselves requesting additional compensation. For some ASCs, this is a request they are grappling with for the first time. It is very important to understand that these arrangements are set at fair market value from a compliance perspective. To help navigate these arrangements, VMG Health has outlined some important factors for ASCs to consider.
When establishing an arrangement for coverage to be supplied by an anesthesia group, it is important for ASCs to understand what level of coverage they will need. This includes a consideration of on-site time needed versus off-site or on-call time. Additionally, it is important to establish the need for medical directorship or other administrative services with a provider group, including an expectation of hours for these roles.
Facilities should consider what types of providers are needed and should confirm with the provider group that this level can be supplied. Leaning on certified registered nurse anesthetists (CRNAs) can be beneficial from a cost perspective for both the provider group and the facility, but the facility should ensure the mix is appropriate for the coverage needed. As provider compensation is typically the largest expense driver in coverage arrangements, it is, of course, important to ensure the right level of expertise is provided. However, the ability to lower provider expenses by leaning on CRNAs should not be overlooked.
As the industry continues to shift towards value-based care, certain quality incentives may be considered for inclusion in a coverage arrangement. Facilities contemplating adding these types of metrics should push for outcomes-based metrics that the providers will have the ability to demonstrably impact. Additionally, facilities should ensure that accurate tracking of outcomes is possible and that targets require the attainment of higher quality versus maintenance of current outcome achievements.
To service a coverage arrangement, provider groups typically will need to incur some additional costs beyond provider comp expenses, including billing and collection expenses and general office support expenses. However, additional requirements might be needed from a facility. Therefore, facilities should work with groups to outline their needs to ensure the provider group is aligned with the expectations under the arrangement beyond the clinical provider requirements.
The No Surprises Act is a major step towards protecting patients from unexpected medical bills, but it presents significant challenges for healthcare providers. Providers must adapt to the new law’s requirements, which can be time-consuming, costly, and complicated. While providers will need to be proactive in addressing these challenges, facilities may be asked to provide further financial assistance in certain arrangements. Having open and thorough conversations about the needs of the facility, while balancing the challenges faced by anesthesia groups, will be an effective way for facilities and providers to continue partnering to provide high-quality care for patients.
January 26, 2023
Written by Jack Hawkins, Ryan Mendez, and Colin Park, CPA/ABV, ASA
The following article was published by Becker’s ASC Review
2022 saw a continuation of 2021 trends as the healthcare industry further rebounded from the coronavirus (COVID-19) pandemic. The Ambulatory Surgery Center (ASC) subindustry largely recovered in 2021, but certain specialties that lagged in 2021 saw a further recovery in 2022. The ASC industry continued to consolidate throughout 2022 despite not having the major platform-level transactions that were observed in 2021. There were trends that started pre-pandemic that continued to be observed in 2022 such as the shift of higher-acuity procedures from the inpatient setting to the outpatient setting, consolidation of ASCs by management companies, and a push by hospitals to grow their ambulatory footprint with a particular focus on the outpatient setting.
Along with these recurring trends, the subindustry was impacted by macroeconomic trends related to upward pressure on labor, supply, and general costs resulting from a tight labor market and elevated inflationary pressures. The continued trend of increased Medicare reimbursement rates saw its largest escalation ever as a direct result of these pressures.
In March 2020, the world was impacted by the spread of the COVID-19 pandemic, and subsequently, 2021 was a year of rebuilding and recovering from the lasting effects brought on by the pandemic. ASCs in 2021 had an increase in case volumes across almost all specialties. This was primarily due to patients who were willing to resume elective procedures that were postponed and centers that kept their doors open.
In 2022, ASCs saw case volume return to pre-pandemic levels or experienced continued growth if they had not already experienced a return to normal operations. Specialties that were hit especially hard by COVID-19, such as ENT, returned to pre-COVID levels in 2022 as schools and school activities returned to pre-pandemic normalcy. In 2022, the impact of the pandemic on ASCs was less related to revenue and more related to expenses. The lingering effects of COVID-19 were related to the shortage of healthcare workers and the supply chain issues that continued to pressure the profitability of surgery centers. Looking into 2023, controlling labor and supply costs will be a point of focus for ASCs.
The trend of higher-acuity procedures shifting from an inpatient or HOPD setting to a freestanding ASC setting continued throughout 2022. In 2022, specialties that increased their footprint in ASCs included cardiology, orthopedics, and higher-acuity spine procedures. According to data from the ASC Association, orthopedics was the most common specialty serviced by ASCs in 2022.
Director of ASC Operations at Virtua Health Catherine Retzbach said ASCs that perform these high acuity cases “offer patients more options to have procedures be performed in a high-quality, low-cost environment.” Furthermore, according to the most recent Ambulatory Surgery Center report published by Research and Markets, ASCs are projected to perform half of all cardiology procedures by the mid to late 2020s.
The ASC subindustry continues to focus on higher-acuity specialties when considering both organic growth and M&A opportunities. President of Tenet Saum Sutaria noted the continued focus of the ASC business toward higher-acuity service lines in the company’s Q3 2022 earnings call. Tenet is the parent company of USPI and is the largest outpatient surgery center operator in the United States. The company reported that these procedures made up 20% of USPI’s year-to-date volume due to growth in their orthopedic and spine business. Sutaria further said “the [USPI] team is focused on organic growth, [and] increase in higher-acuity services and M&A.” These insights highlight the ASC subindustry’s focus on higher-acuity service lines, and indicate the shift towards ASCs for these types of procedures is likely to continue in the future.
In 2022, we saw the continued expansion of a prominent large-level ASC platform player highlighted by the finalization of a large platform-level transaction that began in 2020. In addition, there were a significant number of transactions at the individual-facility level. Consistent with the observed larger platform-level transaction, the fragmented ASC industry has continued to consolidate. It is worth noting that although the industry continues to consolidate approximately 70% of ASC facilities remain independent as of 2022. This leaves room for further consolidation at the individual-facility level.
In 2020, Tenet Health finalized a deal for $1.1 billion to acquire 45 ASCs from SurgCenter Development. This was the first stage of a multi-part acquisition, and in Q4 of 2021, USPI entered a $1.2 billion deal to acquire SurgCenter Development’s remaining centers and established a long-term development deal. The transaction included acquiring ownership interest in an additional 92 ambulatory surgery centers, other support services in 21 states, and providing continuity for future de novo development projects. In 2022, USPI made substantial strides in consolidating the 92 ASCs it acquired from SurgCenter Development. This process is expected to continue into 2023 as the centers are further consolidated. The acquisition has enabled Tenet and USPI to expand their footprint and solidify their position as a leader in the ambulatory surgery center market.
“There’s anticipated additional synergies related to the SCD transactions that will continue to grow as we move through next year as well. And the other thing is the M&A activity that USPI will execute on. The pipeline is robust.”
-Dan Cancelmi, Chief Financial Officer
On June 21, 2022, USPI and United Urology Group formed a joint venture partnership in 22 ASCs. USPI acquired a portion of United Urology Group’s ownership interests in ASCs located in Maryland, Colorado, and Arizona. The ASCs will be owned and operated by the joint venture, and USPI will provide management and support services to the ASCs. The transaction closed in the third quarter. In February 2022 The Rise Fund, an impact investing strategy managed by TPG, announced the acquisition of Blue Cloud Pediatric Surgery Centers which is the largest operator of pediatric dental ASCs in the United States. TPG Rise is a large impact investing platform with more than $13 billion in assets across its various funds, including The Rise Funds, TPG Rise Climate, and the Evercare Health Fund.
On December 9, 2022, Michigan-based Sparrow Health System and Michigan Medicine, formerly the University of Michigan Health System, announced an $800 million partnership. Michigan Medicine will invest $800 million into the expansion of Sparrow’s ASC and neonatal care unit.
In April 2022, UnitedHealth Group’s Optum announced the purchase of Kelsey-Seybold, a Houston-based physician group for $2 billion. The acquisition expanded Optum’s presence in the primary care market. As part of this acquisition, Optum gained two ASCs that were owned by Kelsey-Seybold.
Finally, on May 3, 2022, Surgery Partners and ValueHealth announced a partnership that aims to construct new ASCs and implement ValueHealth’s value-based surgical programs at Surgery Partners’ existing and upcoming locations. Additionally, Surgery Partners will manage and take over ValueHealth’s stake in three current ASCs and four centers that are in the development phase.
As of December 31, 2022, the largest operators (in terms of the number of ASCs) are United Surgical Partners International (USPI), Envision Healthcare/Amsurg Corporation, and Surgical Care Affiliates (SCA), with ownership of approximately 440+, 260+, and 260+ ASCs, respectively.
As noted in the chart below, the number of total centers under partnership by a national operator, as a percentage of total Medicare-certified centers, saw an increase from 2021 to 2022 growing from approximately 1,752 centers to 1,804 centers. Additionally, the top five management companies have increased the number of centers under management by approximately 511 centers since 2011 which represents a compound annual growth rate of 5.37%. As management companies have increased in size they are able to increasingly provide a greater level of strategic value by bringing greater leverage with commercial payors, enhanced management and reporting capabilities, and improved efficiency related to staffing, supplies procurement, and other general and administrative expenses.
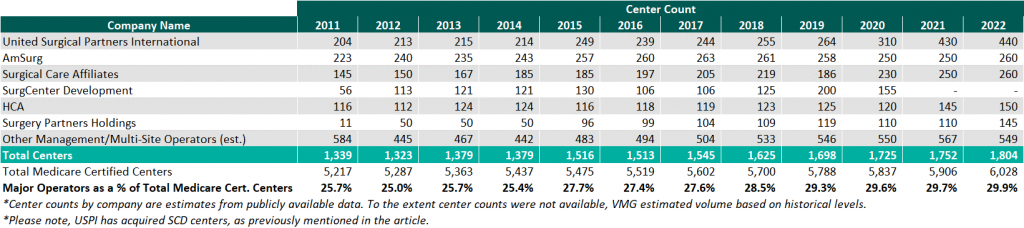
On November 2, 2021, the Medicare reimbursement fee schedule for ASCs in 2022 was finalized by the Centers for Medicare & Medicaid Services (CMS). Consistent with previous years for CYs 2019 through 2023, CMS will update the ASC payment system using the hospital market basket update instead of the Consumer Price Index for All Urban Consumers (CPI-U). CMS published the 2021 ASC payment final rule which resulted in overall expected growth in payments equal to 2.0% in CY 2022. This increase is determined based on a hospital market basket percentage increase of 2.7% less the multifactor productivity (MFP) reduction of 0.7% mandated by the ACA.
Moreover, the ASC payment final rule for CY 2023 was released by CMS on November 1, 2022, and resulted in overall expected growth in payments equal to 3.8% in CY 2023. This increase is determined based on a projected inflation rate of 4.1% less the MFP reduction of 0.3% mandated by the ACA. The 3.8% growth in payments represents the largest increase in projected payments year over year and is a direct result of the increase in labor, supplies, and other cost pressures seen over the last year. Although the industry recognizes the increase in payments as a win, many major players believe the increase was insufficient given the extraordinary cost pressures hospitals and ASCs are facing. The way ASCs navigate the dynamic macroeconomic environment currently in place will be a major point of interest over the coming years.
The table below reflects a summary of the estimated Medicare ASC payments for 2022 and 2023 for the top 10 CPT codes performed in ASCs in 2022. As noted below, the observed 2022 payments by Medicare for the top 10 CPT codes are projected to increase by 3.9% through the estimated 2023 payments.
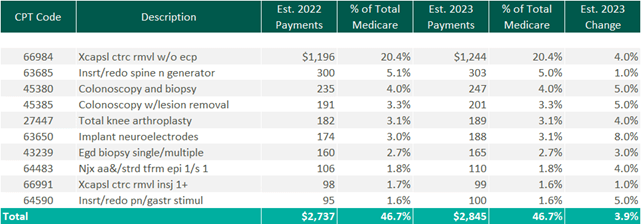
CMS has implemented a new policy that will provide complexity adjustments for certain ASC procedures in CY 2023. These adjustments will be applied to combinations of primary procedures and add-on codes deemed eligible under the hospital outpatient prospective payment system (OPPS). In the past, add-on codes did not receive additional reimbursement when bundled with primary codes. However, with this new policy Medicare will provide adjustments to the payment rate for certain primary procedures to account for the additional cost of performing specific add-on services.
CMS considered 64 recommendations for new procedures to be added to the ASC CPL for CY 2023. After reviewing the clinical characteristics of these procedures, four were chosen to be added to the CPL for the upcoming year. These procedures are typically performed in outpatient settings and have little to no inpatient admissions. The four procedures are outlined in the table below. However, the addition of only four codes resulted in pushback and a continued desire for additional procedures to be added to the CPL that is being performed safely and successfully by ASCs.
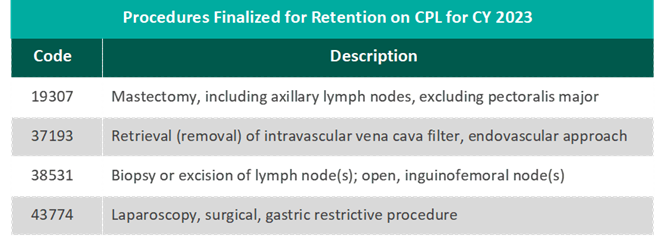
“CMS’s decision to add only four new procedures to the ASC-CPL for 2023 after ASCA proposed 47 procedures that ASCs are performing safely and successfully for privately insured patients is a serious mistake and denies beneficiary access to high-value care. Forcing otherwise healthy Medicare beneficiaries to receive care in higher-cost settings for these procedures needlessly increases costs to the Medicare program and undercuts Medicare’s mission of serving as a responsible steward of public funds.”
– Bill Prentice, Chief Executive Officer, ASCA
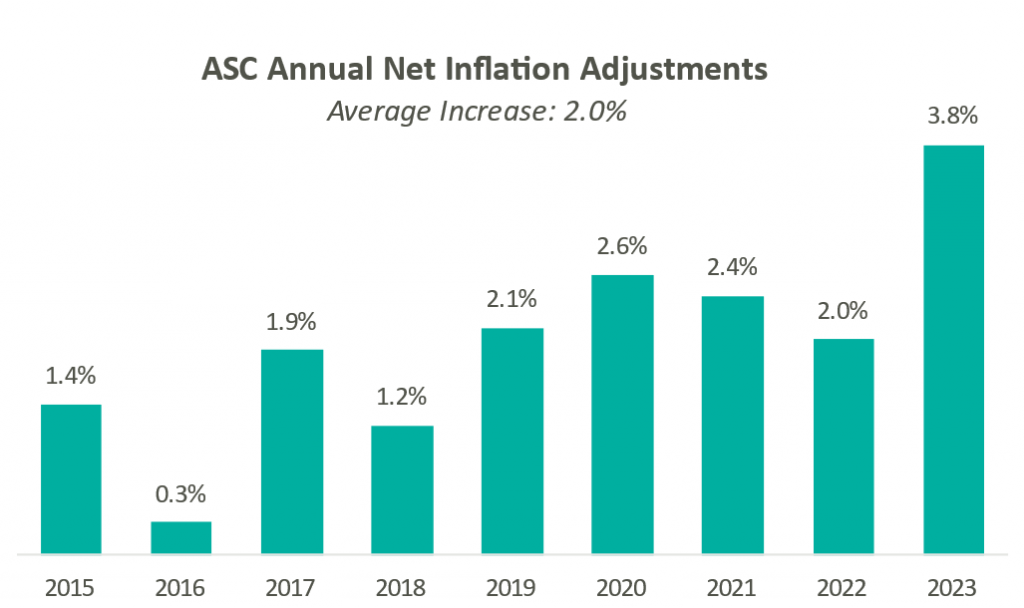
Presented in the chart to the right is a summary of the historical net inflation adjustments for CY 2015 through CY 2023. The annual inflation adjustments are a presented net of additional adjustments, such as the MFP reduction, outlined in the final rule for the respective CY. The CY 2023 inflation adjustment is nearly double the increase we have observed in each of the last eight years and is largely driven by labor and supply cost pressures.
Overall, the final ruling to increase ASC payments by CMS and the increased recovery from COVID-19 both indicate an expected increase in total ASC payments. Ultimately, CMS has projected total ASC payments in 2023 to increase by approximately $230 million from 2022 payments to approximately $5.3 billion.
In conclusion, 2022 was a year of growth throughout the ASC industry and a year of continued recovery from the effects of the pandemic. Key trends to look for going forward are the effects of increased cost pressures impacting the healthcare industry as a whole, and specifically how ASCs respond. Expectations for 2023 are continued growth and consolidation in this sub-industry. The ASC setting provides a convenient, cost-effective way for patients to receive high-quality care. The continued shift of higher-acuity procedures to the outpatient setting should give optimism to the success of the subindustry as a whole as long as cost pressures are mitigated properly. Overall, ASCs at the center level are expected to continue the positive momentum that persisted in 2022 and the subindustry is expected to see the level of transactions increase through 2023.
December 15, 2022
By: Madi Whyde, Savanna Ganyard, CFA, Jordan Tussy, and Madison Higgins
VMG Health reviewed the earnings calls of publicly traded healthcare operators that reported earnings for the third quarter that ended on September 30, 2022. By focusing on the major players in select subsectors defined below, we analyzed the frequency of certain keywords including inflation, COVID-19, interest rates, premium labor, and others. We used these keywords to identify which topics commanded the room this earnings season. Highlights from the calls are summarized in this article.
Volume: Although volume trends are unique to each industry sector nearly all operators remained focused on the impacts of COVID.
Poll: Did the earnings call mention COVID-19?
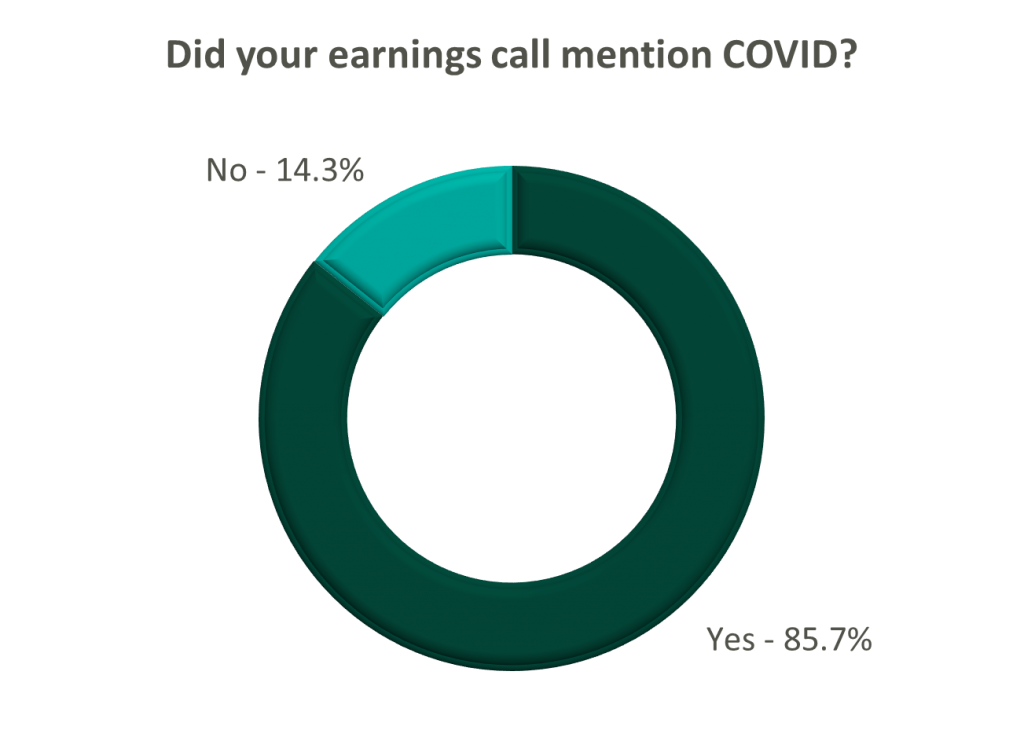
On a same-facility basis, admission volumes declined as much as 5.0% from the comparable prior year quarter (Q3 2021) for acute care hospital operators. Despite the weakening of COVID-19, the decline in volumes was attributed to higher-than-average cancellation rates (THC), the migration of certain procedures to outpatient status (CYH and HCA), and capacity constraints (HCA). Inpatient volumes generally remained at or below pre-pandemic levels.
Ambulatory surgery center (ASC) operators reaped the benefits of the migration to the outpatient setting and reported positive volume trends when compared to Q3 2021. Surgical volumes were reported as consistent with 2019 pre-pandemic levels (THC), and one operator claimed the business did not experience any material direct impact related to COVID-19 during Q3 2022 (SGRY).
The post-acute sector reported mixed results in volume trends. One operator reported a year-over-year decline of 14.0% in hospice admissions, citing capacity constraints and reduced referrals from acute care hospitals (EHAB). However, another operator indicated that increases in admissions in the second half of the third quarter showed growth that they “haven’t experienced since the start of the pandemic” (CHE).
Volume trends among other industry players including dialysis providers, risk-bearing organizations, and physician services were also affected by COVID-19 in Q3 2022. Headwinds in dialysis volumes are expected to persist for the foreseeable future (DVA), and inpatient volumes for risk-bearing organizations remain below pre-pandemic levels (AGL). Notably, AGL also reported a rebound in physician office visits and outpatient volumes were in line with pre-pandemic levels.
Reimbursement: Declining COVID-19 volumes mean less incremental government revenue for certain industry players who also now contend with an uncertain inflationary environment.
Poll: Did the earnings call mention inflation?
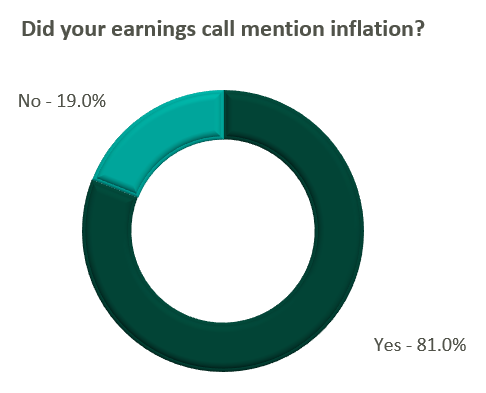
Declining COVID-19 volumes resulted in lower acuity patients and reduced incremental government reimbursement. This softened the reimbursement per admission for the acute care hospital segment. Further exacerbated by inflation, these dynamics were evident in reported EBITDA margins which declined as much as 17.0% (CYH) over Q3 2021. In response, some acute care hospital operators are turning to commercial payor negotiations. Rate increases for the next year are anticipated to range from a minimum of 3.0% (THC) to upwards of 6.0% (CYH).
The post-acute sector did not release specific figures regarding contract rate hikes. However, the sector is optimistically looking for high single-digit rate increases (SEM) to provide relief in the current inflationary environment.
Labor: Unsurprisingly, management teams across the sector were faced with questions about labor trends and management techniques during their earnings calls. Contract labor remained pivotal for the operations of some, but premium labor appears to have softened during the quarter.
Poll: Did the earnings call mention premium or contract labor?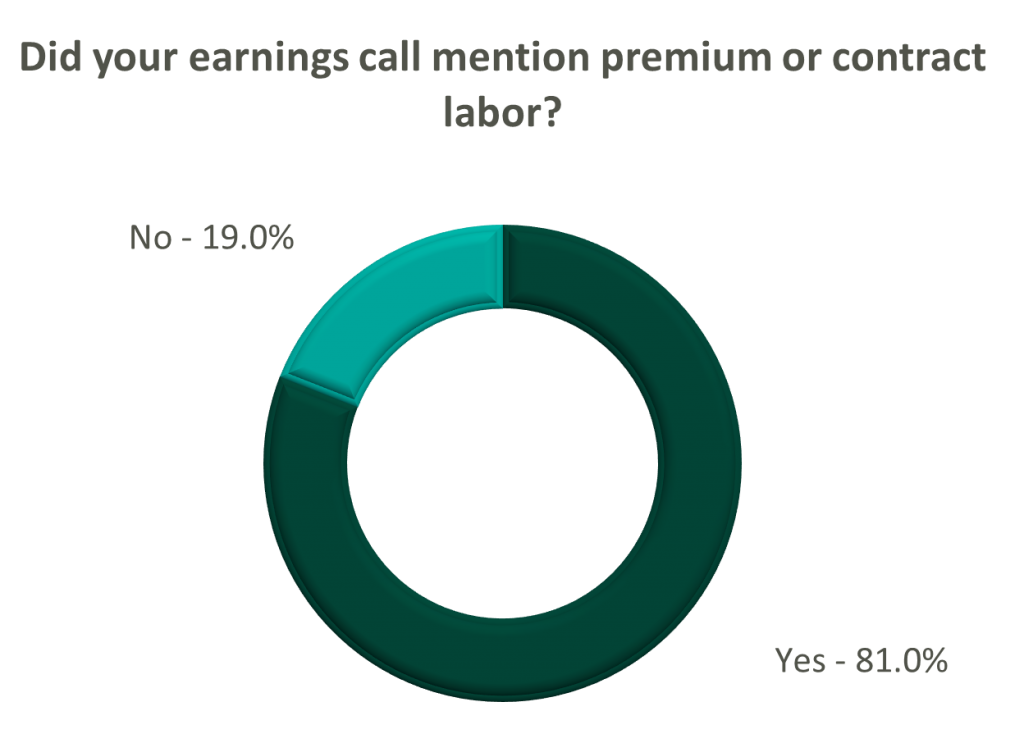
The reliance on contract labor continued its downward trend in Q3 helping moderate expenses. HCA even indicated overall labor costs were stable due to targeted market adjustments. However, contract labor and premium pay remain at uncomfortably high levels for most acute care hospital operators. UHS revealed during their call it will be unlikely to reach pre-pandemic levels in the near future.
Staffing challenges persisted among the post-acute operators and directly impacted volume by as much as 60.0% (AMED). Increased indirect labor costs including orientation, training, and sign-on bonuses were the leading drivers of decreased EBITDA (AMED). Wage inflation, particularly for nursing positions, is expected to rise as much as 5.0% next year (SEM). However, several management teams are optimistic wages will stabilize to historical levels (SEM, EHC) in the near future.
Other industry players, including dialysis and physical therapy providers, also faced challenges with contract labor during the quarter. USPH reported labor costs were approximately 200 basis points higher than Q3 2021 levels, and DVA indicated such costs showed no improvement.
Go Forward Expectations and Guidance: Considering the quarter’s performance, the companies we reviewed were divided relatively evenly in terms of revised FY 2022 revenue guidance, (i.e., raised, lowered, unchanged). In general, the quarter brought about a more pessimistic view of FY 2022 EBITDA, and the majority of public companies lowered their guidance for the year. Further, most stakeholders were left with no guidance for FY 2023.
Poll: Did the earnings call mention a recession?
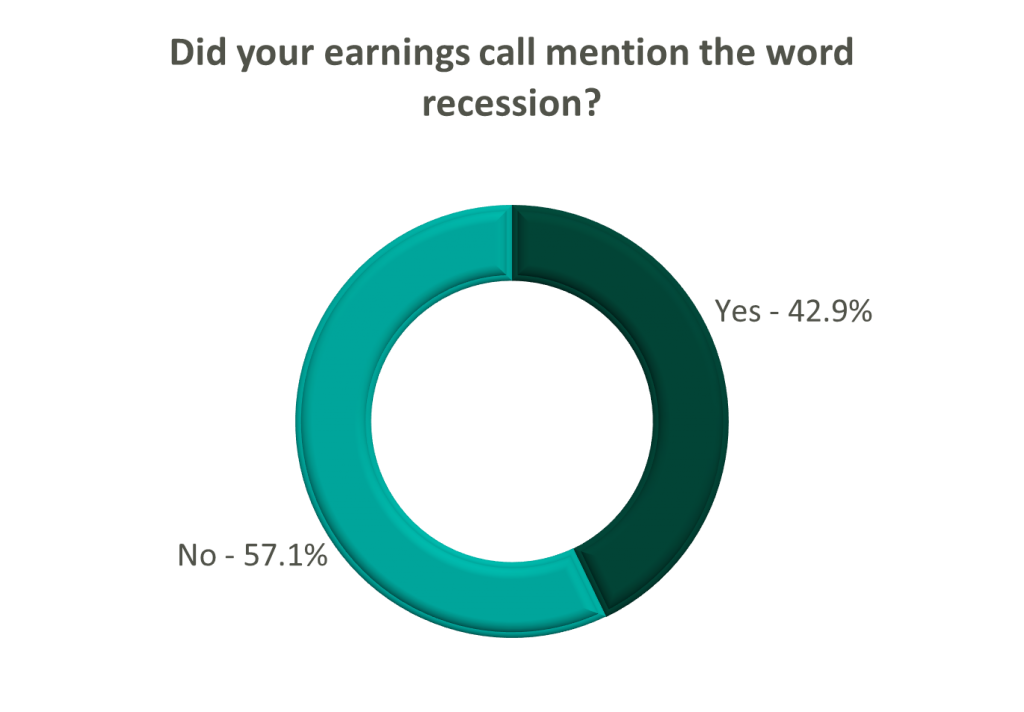
FY 2022 revenue and EBITDA guidance among the acute care hospital operators was generally left unchanged except for THC which lowered EBITDA guidance. However, all companies that were reviewed declined to provide FY 2023 guidance during the call, and primarily cited economic uncertainty (HCA).
The post-acute sector appeared nearly unanimous in the outlook for the rest of 2022, and most operators lowered their revenue and EBITDA guidance. Unsurprisingly, no one offered FY 2023 guidance during the earnings calls.
Interestingly, risk-bearing organizations mostly raised their revenue guidance for FY 2022 (AGL, CMAX, PRVA). However, EBITDA guidance was less predictable and was lowered (AGL, TOI), raised (PRVA), and unchanged (CMAX).
Most other healthcare operators followed similar patterns in terms of providing guidance for FY 2023. Of the companies we reviewed, only DVA revealed an outlook for the next year. The company anticipates revenue to be flat (driven by unfavorable volume trends) and margins to continue to feel the impact of labor market pressures.
Related Content